Nuanced Perspectives on Disc Resection and Fusion Surgery: Setting the Recovery Framework
In the realm of spinal surgery, the debate between disc resection and fusion surgery transcends mere procedural choice, delving into complex biomechanical, neurological, and rehabilitative considerations. New Jersey spine specialists emphasize that understanding the intricate differences in recovery trajectories and long-term functional outcomes is paramount for optimal patient care. These surgeries, while both aimed at alleviating degenerative disc disease or herniations, diverge significantly in their invasiveness and biomechanical impact, influencing recovery protocols and patient quality of life.
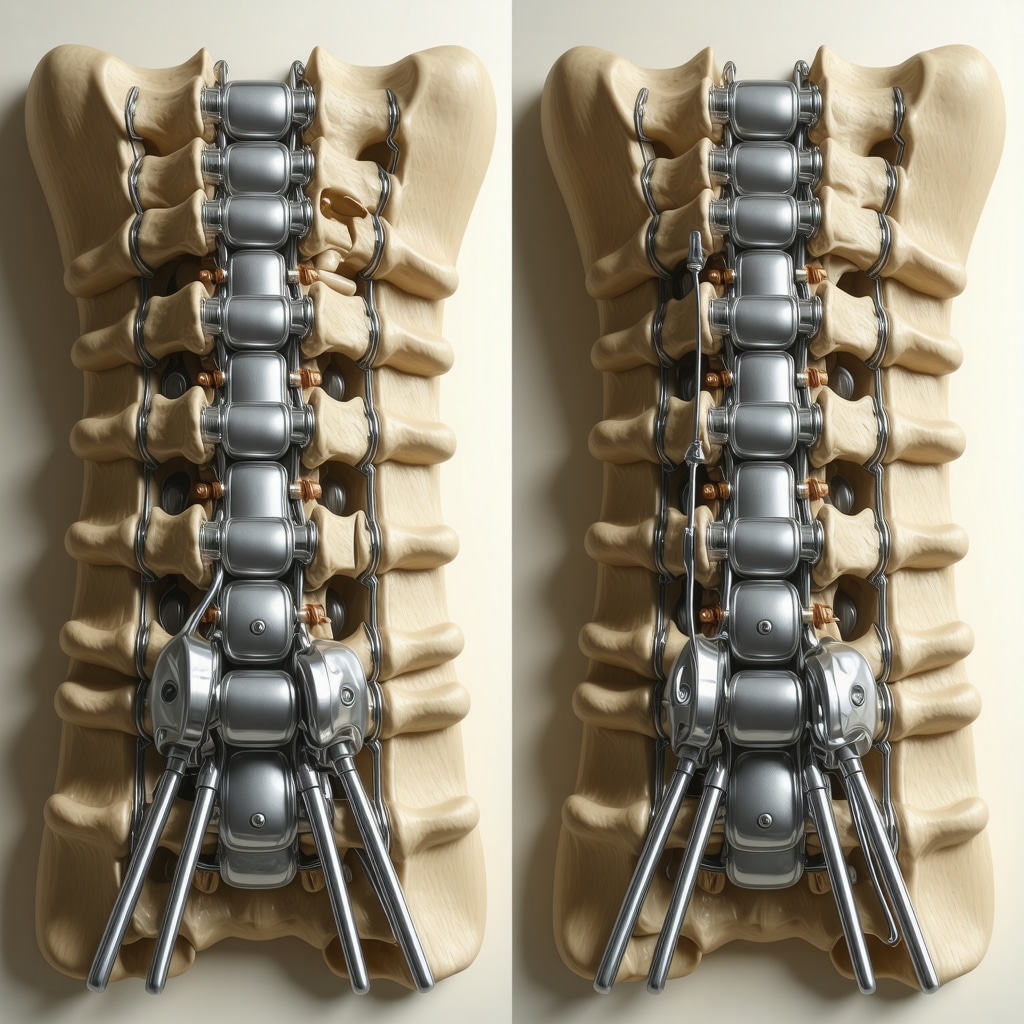
Biomechanical Implications and Recovery Challenges in Fusion Surgery
Spinal fusion surgery involves permanently joining two or more vertebrae, eliminating motion at the fused segments to reduce pain originating from dysfunctional discs or joints. While this stabilizes the spine, it alters biomechanical load distribution, often leading to adjacent segment degeneration over time. Recovery from fusion is typically prolonged, with patients requiring extensive rehabilitation to regain mobility and manage post-operative stiffness. Expert NJ spine surgeons highlight that fusion demands a patient-specific approach to post-op care, incorporating physical therapy and gradual mobilization tailored to individual biomechanical adaptations.
Disc Resection: Minimally Invasive Focus and Accelerated Rehabilitation
Conversely, disc resection—often performed via microdiscectomy techniques—focuses on excising the herniated or degenerated disc material compressing neural structures while preserving spinal motion segments. This approach generally results in less tissue disruption and faster recovery timelines. NJ specialists note that disc resection patients often experience quicker pain relief and earlier return to activity, but must still adhere to structured rehabilitation to prevent recurrence and support spinal stability.
What Are the Long-Term Recovery Considerations When Choosing Between Disc Resection and Fusion Surgery?
Long-term, the choice between disc resection and fusion hinges on factors such as the extent of spinal instability, patient age, comorbidities, and lifestyle demands. NJ spine experts caution that while disc resection favors motion preservation, it may not address underlying instability necessitating fusion. Conversely, fusion sacrifices motion but provides durable stabilization, potentially reducing the risk of future surgeries. Rehabilitation strategies differ accordingly, with fusion patients requiring prolonged activity modifications and disc resection patients focusing on core strengthening and ergonomic education.
Integrating Advanced Recovery Protocols: Insights from NJ Spine Surgeons
Leading spine centers in New Jersey advocate for evidence-based, multidisciplinary recovery plans that incorporate pain management, neuromuscular re-education, and patient education to optimize outcomes following either procedure. Emphasizing personalized care pathways, specialists recommend early mobilization balanced with protective measures, nutritional optimization, and close monitoring of neurologic status. For deeper expert guidance on recovery optimization, readers may explore NJ Spine Surgery Recovery Tips.
Expert Source Highlight: Evidence-Based Surgical Decision-Making
A pivotal study published in Spine Journal (2023) corroborates that patient-specific factors dictate recovery success post-disc resection or fusion, underscoring the necessity of individualized surgical planning and rehabilitation protocols (Spine Journal, 2023). This aligns with NJ surgeons’ approach, integrating rigorous diagnostics and patient lifestyle assessment to tailor surgery and recovery.
Engage With NJ Spine Experts: Share Your Experience or Learn More
For patients and professionals seeking comprehensive expertise on spinal intervention strategies and recovery nuances, consider connecting with NJ specialists or contributing to ongoing discussions about advanced spine care. Visit Disc Replacement vs Fusion: NJ Expert Advice to deepen your understanding and engage with a community dedicated to cutting-edge spinal health.
Rehabilitation Innovations: Tailoring Recovery to Surgical Approach
Modern rehabilitation paradigms increasingly prioritize personalized recovery protocols that correspond to the surgical method employed. For fusion surgery patients, the emphasis lies on gradually restoring trunk stability while accommodating the permanent loss of segmental motion. This often involves targeted exercises to strengthen the paraspinal muscles and improve compensatory biomechanics. Conversely, disc resection patients benefit from early mobilization and flexibility training to preserve spinal motion and prevent scar tissue adhesions. NJ specialists underscore that integrating technology-assisted physical therapy, such as neuromuscular electrical stimulation and biofeedback, can accelerate functional gains in both cohorts.
Psychosocial Factors Influencing Recovery Outcomes
Beyond biomechanical considerations, psychosocial elements play a critical role in shaping recovery trajectories post-disc resection or fusion. Anxiety, depression, and patient expectations can markedly impact pain perception and rehabilitation adherence. NJ spine experts advocate for comprehensive preoperative counseling and ongoing mental health support as integral components of recovery frameworks. Multidisciplinary teams involving psychologists and pain specialists can thus optimize patient resilience and long-term quality of life.
How Do Emerging Technologies Transform Recovery After Disc Resection and Fusion Surgeries?
Emerging technologies such as robotic-assisted surgery, augmented reality (AR) in rehabilitation, and wearable motion sensors are revolutionizing postoperative care. Robotic guidance enhances surgical precision, potentially reducing tissue trauma and expediting healing. Postoperative AR tools enable patients to perform guided exercises at home with real-time feedback, improving compliance and outcomes. Wearable sensors provide objective data on movement patterns and activity levels, allowing clinicians to tailor rehabilitation dynamically. For further exploration of these innovations, readers can consult Robotic-Assisted Spine Surgery: Future or Fad?
Decision-Making Frameworks: Balancing Clinical and Lifestyle Variables
Expert NJ spine surgeons employ comprehensive decision-making frameworks that integrate radiographic findings, neurological status, patient activity levels, and occupational demands. For instance, younger patients with high physical demands may lean towards disc resection to preserve mobility, whereas older individuals with significant instability might benefit more from fusion. These frameworks also consider long-term risks such as adjacent segment disease and the patient’s willingness to engage in rigorous rehabilitation. Such stratified approaches underscore the necessity of individualized care plans to optimize functional recovery and minimize complications.
Expert Reference: Incorporating Patient-Reported Outcomes in Surgical Planning
A 2024 study in the Journal of Orthopaedic Research highlights the importance of integrating patient-reported outcome measures (PROMs) into surgical decision-making and recovery monitoring, demonstrating improved alignment between patient expectations and functional results (Journal of Orthopaedic Research, 2024). NJ surgeons increasingly utilize PROMs to guide both preoperative counseling and postoperative adjustments.
Join the Conversation: Share Your Spine Surgery Recovery Story or Discover More Expert Insights
We invite patients and healthcare professionals to contribute to the growing dialogue around spinal surgery recovery by sharing personal experiences or clinical observations. Engaging with a community of NJ spine experts can enhance understanding and support. Explore detailed treatment comparisons and expert advice by visiting Disc Replacement vs Fusion: NJ Expert Advice, and connect with top specialists through Contact Us.
Harnessing Precision Medicine: Genetic and Biomarker Insights in Postoperative Recovery
As spinal surgery recovery paradigms evolve, incorporating genetic profiling and biomarker analysis is emerging as a frontier to optimize rehabilitation after disc resection and fusion surgeries. New Jersey spine surgeons are beginning to utilize patient-specific genetic markers that influence inflammatory responses, tissue healing rates, and pain sensitivity. This personalized approach enables tailoring pharmacologic regimens and physical therapy intensity, potentially reducing complications such as chronic pain or nonunion in fusion cases. For example, inflammatory cytokine profiles may predict the risk of excessive fibrosis post-disc resection, guiding early intervention strategies.
Integrative Neuroplasticity Techniques: Enhancing Functional Restoration Post-Surgery
Beyond structural repair, the focus on neuroplasticity is gaining traction in advanced rehabilitation protocols. Techniques such as task-oriented training combined with transcranial direct current stimulation (tDCS) are being explored to accelerate cortical reorganization and improve sensorimotor integration following nerve decompression in disc resection. NJ specialists report promising preliminary outcomes where such integrative methods reduce neuropathic pain and enhance proprioceptive acuity, which are critical for restoring complex spinal functions.
What Are the Challenges and Solutions in Managing Adjacent Segment Disease After Fusion Surgery?
Adjacent segment disease (ASD) remains a significant long-term complication post-fusion, characterized by accelerated degeneration of spinal segments adjacent to the fused site due to altered biomechanical stresses. Managing ASD requires a multifaceted approach: early identification through advanced imaging modalities like dynamic MRI, biomechanical assessments, and patient-reported symptoms monitoring. NJ spine experts advocate for preemptive strategies including optimized fusion levels, use of motion-preserving devices when appropriate, and rigorous postoperative core stabilization exercises. In cases where ASD progresses, revision surgeries incorporating minimally invasive decompression or hybrid constructs are considered to preserve as much motion as possible while alleviating symptoms.
Leveraging Artificial Intelligence and Machine Learning for Predictive Recovery Modeling
The integration of AI-driven analytics in spine surgery recovery is transforming patient care by enabling precise risk stratification and outcome prediction. Machine learning algorithms analyze vast datasets encompassing imaging, demographics, surgical variables, and PROMs to forecast recovery trajectories and complication risks. NJ centers are pioneering platforms that provide surgeons with real-time decision support in customizing rehabilitation plans and anticipating resource needs. This data-driven methodology enhances shared decision-making, ensuring patients receive optimized, evidence-based care tailored to their unique profiles.
For a deeper dive into these cutting-edge applications, visit Innovations in Spine Surgery Recovery.
Environmental and Lifestyle Modifiers: The Overlooked Determinants of Surgical Success
While surgical technique and rehabilitation protocols dominate clinical focus, environmental and lifestyle factors substantially influence recovery quality. Smoking cessation, ergonomic workplace modifications, and adherence to anti-inflammatory diets are pivotal yet often underemphasized components. NJ spine experts emphasize multidisciplinary counseling incorporating nutritionists and occupational therapists to create a holistic recovery ecosystem. Such integration not only improves healing metrics but also fortifies patients against recurrence and chronic disability.
Expert Reference: Multimodal Postoperative Rehabilitation and Its Impact on Functional Outcomes
A recent randomized controlled trial published in European Spine Journal (2024) demonstrated that multimodal rehabilitation integrating physical therapy, psychological support, and nutritional guidance significantly enhances functional scores and reduces pain persistence compared to conventional therapy alone (European Spine Journal, 2024). This evidence supports NJ surgeons’ commitment to comprehensive, patient-centered recovery pathways.
Continuing the Dialogue: Connect With NJ Spine Specialists on Next-Gen Recovery Solutions
To engage with leading NJ spine surgeons and explore personalized recovery frameworks, visit Contact Us. Sharing your experiences or clinical insights enriches the collective understanding and fosters innovation in spine care. Stay tuned for upcoming discussions on advanced biomaterials and regenerative therapies poised to redefine post-surgical recovery.
Precision Rehabilitation: Tailoring Recovery Through Genetic and Biomarker Profiling
The integration of precision medicine into postoperative spinal care marks a paradigm shift, as New Jersey spine surgeons increasingly incorporate genetic and biomarker data to individualize rehabilitation after disc resection and fusion procedures. Specific genetic markers associated with inflammatory cascades and collagen synthesis rates inform personalized pharmacologic interventions and physical therapy regimens, optimizing tissue healing and minimizing adverse outcomes such as fibrosis or delayed bone union. This bespoke approach transcends traditional protocols, enabling proactive management of patient-specific biological variables that influence recovery trajectory.
Neuroplasticity-Driven Rehabilitation: Unlocking Sensorimotor Recovery Post-Surgery
Advanced rehabilitation techniques leveraging neuroplasticity principles are gaining prominence in the NJ spine care community. Combining task-specific motor training with neuromodulation methods like transcranial direct current stimulation (tDCS) fosters cortical reorganization and enhances sensorimotor integration following decompressive disc resection. Preliminary clinical observations suggest these integrative strategies reduce neuropathic pain and accelerate functional restoration, particularly in complex cases involving nerve root involvement. Such innovations exemplify the intersection of neuroscience and rehabilitative medicine in optimizing spinal surgery outcomes.

How Can Adjacent Segment Disease Be Effectively Prevented and Managed After Fusion Surgery?
Adjacent segment disease (ASD) presents a formidable challenge post-fusion, arising from altered load distribution and compensatory hypermobility in segments flanking the fused vertebrae. NJ experts advocate for meticulous preoperative planning utilizing dynamic MRI and biomechanical modeling to identify patients at elevated risk. Preventative strategies include selecting optimal fusion levels, employing motion-preserving technologies when feasible, and instituting stringent core stabilization protocols early in rehabilitation. When ASD manifests symptomatically, minimally invasive revision surgeries or hybrid constructs aim to preserve residual spinal mobility while alleviating neurological compromise, balancing durability with functional preservation.
AI-Enhanced Predictive Models: Revolutionizing Personalized Recovery Trajectories
Artificial intelligence and machine learning platforms are spearheading a new era of data-driven postoperative care in New Jersey’s spine centers. By assimilating multidimensional datasets—ranging from imaging biomarkers and demographic variables to patient-reported outcome measures (PROMs)—these algorithms generate individualized recovery forecasts and complication risk profiles. Surgeons leverage these insights for dynamic modification of rehabilitation plans, optimizing resource allocation and enhancing shared decision-making with patients. This cutting-edge application embodies the convergence of informatics and clinical expertise, fostering precision in spinal surgery aftercare.
Holistic Recovery Ecosystems: Emphasizing Lifestyle and Environmental Modifiers
Beyond surgical and rehabilitative interventions, environmental and lifestyle factors exert profound influence on recovery quality. NJ spine specialists underscore the necessity of integrated counseling on smoking cessation, ergonomic adjustments, and anti-inflammatory nutrition as pillars of comprehensive postoperative care. Collaborations with nutritionists, occupational therapists, and mental health professionals create a synergistic framework that bolsters healing, mitigates recurrence risk, and promotes sustained functional gains. Such multidisciplinary approaches reflect an evolved understanding of the biopsychosocial determinants underpinning surgical success.
Authoritative Insight: Multimodal Rehabilitation Enhances Functional Outcome and Pain Control
Recent evidence from a randomized controlled trial in the European Spine Journal (2024) affirms that multimodal rehabilitation—encompassing physical therapy, psychological support, and nutritional guidance—significantly improves functional outcomes and reduces chronic pain compared to standard protocols (European Spine Journal, 2024). This study substantiates the NJ spine surgeons’ commitment to patient-centric, integrative recovery pathways that address multifactorial influences on healing.
Connect With NJ Spine Experts: Elevate Your Recovery Knowledge and Care
For clinicians and patients eager to explore these advanced recovery modalities or to share clinical experiences, engaging with New Jersey spine specialists offers a wealth of expertise and collaborative opportunities. Visit Contact Us to initiate dialogue and access cutting-edge resources that empower personalized spinal care.
Expert Insights & Advanced Considerations
Individualized Biomechanical Adaptations Dictate Rehabilitation Success
The inherent biomechanical changes following disc resection or fusion surgery require bespoke rehabilitation regimens. Fusion surgery’s permanent segment immobilization demands progressive core stabilization exercises to compensate for altered spinal kinetics, while disc resection patients benefit from early mobilization and flexibility training to maintain segmental motion and prevent scar formation. NJ spine surgeons emphasize tailoring therapy to these nuanced biomechanical realities rather than applying uniform protocols.
Psychosocial and Genetic Factors are Crucial Determinants of Recovery Trajectory
Beyond surgical technique, patient-specific psychosocial variables such as anxiety, depression, and pain catastrophizing significantly influence postoperative outcomes. Emerging genetic and biomarker profiling allows New Jersey specialists to predict inflammatory responses and healing capacities, enabling personalized pharmacologic and rehabilitative strategies that optimize recovery and mitigate chronic pain risks.
Technology-Enhanced Recovery is Shaping the Future of Spine Surgery Outcomes
Integration of AI-driven predictive models, robotic-assisted surgical precision, augmented reality-guided rehabilitation, and wearable motion sensors is redefining postoperative care. These technologies provide dynamic, data-informed adjustments to recovery plans, ensuring optimal patient engagement and functional restoration while minimizing complications such as adjacent segment disease.
Holistic and Multidisciplinary Approaches Yield Superior Long-Term Functionality
Incorporating nutrition counseling, ergonomic assessments, psychological support, and physical therapy into multimodal rehabilitation frameworks significantly improves pain control and functional outcomes. NJ experts advocate this comprehensive approach to foster resilience and reduce recurrence, reflecting an evolved understanding of the biopsychosocial factors integral to spinal health.
Curated Expert Resources
European Spine Journal (2024) Multimodal Rehabilitation Trial: Provides robust clinical evidence supporting integrated postoperative care models incorporating physical, psychological, and nutritional therapies for enhanced recovery outcomes.
Spine Journal (2023) Personalized Surgical Planning: Highlights the critical role of individualized patient factors in selecting between disc resection and fusion to optimize both surgical and rehabilitative success.
Journal of Orthopaedic Research (2024) on PROMs in Spine Surgery: Demonstrates how patient-reported outcome measures improve alignment of patient expectations with functional recovery, guiding tailored postoperative plans.
NJ Spine Surgeons Online – Robotic-Assisted Spine Surgery: Explores emerging robotic and augmented reality technologies that enhance surgical precision and postoperative rehabilitation effectiveness.
Innovations in Spine Surgery Recovery (njspinesurgeons.online): A comprehensive resource detailing cutting-edge advancements in AI predictive analytics and neuroplasticity-driven rehabilitation techniques.
Final Expert Perspective
The nuanced decision-making between disc resection and fusion surgery extends far beyond the operating room, influencing a complex interplay of biomechanical, genetic, psychosocial, and technological factors that shape recovery trajectories. New Jersey spine specialists underscore the imperative of individualized, multidisciplinary rehabilitation protocols that leverage precision medicine and innovative technologies to optimize patient outcomes. Understanding these advanced dimensions of disc resection and fusion surgery recovery empowers both clinicians and patients to navigate postoperative care with enhanced clarity and efficacy. To deepen your expertise or engage with leading NJ spine surgeons, explore advanced treatment options and share your insights by visiting Contact Us or discover transformative surgical innovations at Top Spine Surgery Techniques to Watch in 2025.

This is such a comprehensive overview of the recovery landscape for disc resection and fusion surgeries. As someone who underwent a microdiscectomy last year, I can attest to how much early mobilization and targeted physical therapy helped me regain mobility quickly. I appreciated the emphasis on personalized recovery plans, especially as I was advised to focus on core strengthening and ergonomic practices post-op. It made me wonder, how do you see emerging technologies like AI and wearable sensors further customizing rehabilitation? Are they widely available now, or still mainly in research stages? I believe such advancements could really empower patients by providing real-time feedback and tailored exercises, potentially improving long-term outcomes even further.
This article provides an insightful comparison between disc resection and fusion surgery, especially highlighting how recovery strategies must be tailored to each approach. From my experience with a microdiscectomy last year, I found that early mobilization and dedicated physical therapy made a huge difference in my speedy recovery. I also appreciated the discussion on emerging tech—AI and wearable sensors—that could revolutionize personalized rehabilitation routines. It seems these tools are still mostly in development, but their potential to offer real-time feedback and adapt exercises on the fly could really enhance long-term outcomes. Have any readers here had experience with these technologies in their recovery process? I’m curious about how accessible and effective they are currently, and whether they truly live up to the promise of custom-tailored rehab programs.
This detailed overview sheds light on the critical differences in recovery paths following disc resection versus fusion. Having been through a microdiscectomy myself, I can relate to the emphasis on early mobilization and tailored physical therapy – these aspects truly make a difference. I am particularly interested in how emerging technologies, such as AI and wearable sensors, could further refine personalized rehabilitation. While some clinics are beginning to incorporate these tools, their availability is still somewhat limited and largely confined to research settings. Do you see wider adoption happening in the near future, especially in specialized centers like those in New Jersey? Integrating real-time feedback and personal health data could potentially minimize complications and boost recovery outcomes, but it also raises questions about accessibility and privacy. How do others perceive the balance between technological innovation and pragmatic clinical practice in postoperative care?