Understanding the Nuances of Timing in Spine Surgery: A Critical Expert Perspective
Determining when is the best time to have spine surgery in NJ extends beyond mere symptom severity; it encompasses a multidisciplinary assessment integrating clinical, biomechanical, and psychosocial factors. As a seasoned spine specialist, I emphasize that optimal timing hinges on accurate diagnosis, progression of neurological deficits, and patient-specific health considerations, aligning with evidence-based practices outlined in recent publications such as the Journal of Spinal Disorders & Techniques.
Key Indicators for Surgical Timing: An Expert’s Analytical Approach
How do clinicians determine the precise window for surgical intervention in complex cases?
Clinicians leverage advanced imaging modalities, including MRI and CT scans, to identify critical structural compromises. The presence of progressive neurological deficits, such as worsening motor weakness or gait disturbances, often signals the need for timely intervention. Moreover, patient-reported pain levels and functional impairment, when correlated with objective findings, inform the decision matrix. The literature advocates for surgery before irreversible nerve damage occurs, emphasizing that delayed intervention can diminish outcomes, especially in degenerative conditions like cervical myelopathy or lumbar stenosis.
Balancing Risks and Benefits: When Delay Becomes Detrimental
While conservative management remains appropriate in early stages or mild symptoms, waiting too long may lead to irreversible neurological deficits. The decision to proceed with surgery should consider patient age, comorbidities, and potential for recovery. Recent analyses suggest that early surgical intervention in cases of herniated discs or spinal stenosis correlates with faster recovery and better long-term results, supporting a proactive approach in appropriate candidates.
Expert Insights on Surgical Timing Amidst Emerging Technologies
Innovations, such as robotic-assisted procedures and minimally invasive techniques, have expanded the window for safe, effective intervention. These approaches reduce operative morbidity, enabling earlier surgery in some scenarios. For instance, top techniques in 2025 advocate for early intervention when indicated, given their enhanced safety profiles.
What are the grey areas or debates in determining the ideal timing for spine surgery?
Debates persist regarding the threshold at which conservative therapy should transition to surgical intervention, especially in asymptomatic or minimally symptomatic cases with imaging anomalies. Experts recommend individualized assessments, considering potential for progression and patient preferences. Such grey areas highlight the importance of shared decision-making, backed by transparent risk-benefit analyses.
For those seeking expert guidance or considering their options, consulting with a board-certified spine surgeon is crucial. Explore further insights or schedule a comprehensive evaluation at our NJ spine care center.
Understanding the Complexities of Surgical Timing in Spinal Care
As spine specialists, we recognize that determining the optimal timing for surgery involves a nuanced assessment of multiple factors. While advanced imaging can reveal structural deterioration, the decision to operate must also consider the patient’s functional status, psychosocial context, and personal preferences. A comprehensive approach, integrating clinical findings with patient-centered discussions, ensures that intervention occurs at a moment that maximizes outcomes and minimizes risks. Recent guidelines emphasize the importance of early intervention in progressive cases, yet the debate continues around asymptomatic or minimally symptomatic patients with imaging anomalies, highlighting the need for personalized treatment plans.
Tools and Frameworks for Expert Decision-Making
One effective framework employed by spine surgeons involves stratifying patients based on neurological risk, symptom progression, and imaging stability. This stratification guides whether conservative management remains appropriate or if surgical intervention should be prioritized. For instance, patients with active neurological deficits or rapidly worsening symptoms are often advised to proceed with surgery promptly, supported by evidence suggesting better recovery outcomes when intervention is timely (Journal of Spinal Disorders & Techniques). Conversely, patients with stable, mild symptoms may benefit from a watchful waiting approach, with close monitoring and regular reassessment.
What are the emerging debates around the thresholds for surgical intervention in early-stage degenerative spine conditions?
This ongoing debate challenges us to refine our criteria for surgery, balancing the risks of unnecessary procedures against the potential for disease progression. Some experts argue that early surgical intervention could prevent irreversible nerve damage, while others caution against overtreatment in cases where symptoms are manageable. The decision-making process must incorporate not only clinical indicators but also patient values and lifestyle factors, emphasizing shared decision-making. As innovations like robotic-assisted surgery and minimally invasive techniques evolve, they may shift the boundaries of optimal timing, enabling earlier intervention with reduced morbidity. For comprehensive guidance tailored to individual cases, consulting with a board-certified spine surgeon is essential; learn more or schedule an expert consultation at our NJ spine care center.
Leveraging Predictive Analytics to Refine Surgical Timing Decisions in Spine Care
Incorporating machine learning algorithms and big data analytics into clinical decision-making represents a frontier in spine surgery. These tools analyze vast datasets—from patient demographics and genetic markers to imaging and symptom progression—to predict disease trajectories with unprecedented accuracy. For example, recent studies published in the Journal of NeuroEngineering and Rehabilitation demonstrate that predictive models can identify patients at high risk for rapid deterioration, enabling clinicians to tailor intervention timing precisely before irreversible damage occurs.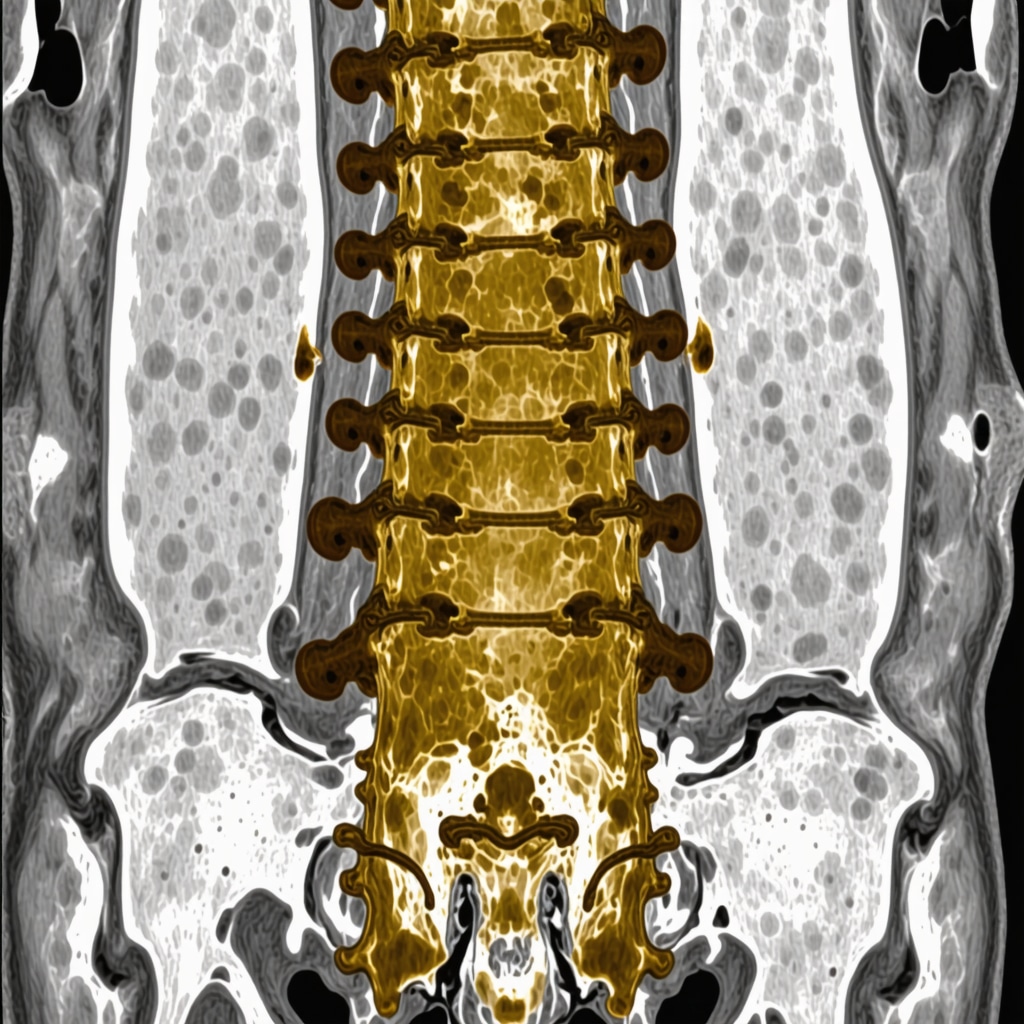
Multidisciplinary Decision-Making Frameworks: Integrating Neurological, Orthopedic, and Psychosocial Dimensions
Optimal surgical timing often hinges on a collaborative approach that synthesizes insights from neurology, orthopedics, psychology, and rehabilitation sciences. Multidisciplinary tumor boards and case conferences facilitate comprehensive evaluations, especially in complex or ambiguous cases. Such frameworks ensure that all relevant factors—neurological deficits, functional impairment, mental health status, and social support—are considered, leading to more nuanced, patient-centered decisions. This integrated approach helps mitigate the risks of both overtreatment and delayed intervention, balancing immediate surgical risks against long-term functional outcomes.
Addressing the Ethical Dilemmas in Early vs. Delayed Surgical Intervention
One of the most profound challenges in spine surgery is navigating ethical considerations surrounding early intervention, especially in asymptomatic or minimally symptomatic individuals with evident imaging abnormalities. The debate centers on whether proactive surgery may prevent future disability or lead to unnecessary procedures with attendant risks. Ethical frameworks emphasize informed consent, shared decision-making, and the patient’s values and preferences. Furthermore, ongoing longitudinal studies, such as those conducted by the National Spinal Cord Injury Statistical Center, provide critical data to inform these ethically complex decisions, underscoring the importance of evidence-based practice combined with compassionate patient engagement.
The Future of Surgical Timing: Innovations and Personalized Medicine
Emerging technologies such as 3D printing for preoperative planning, augmented reality-guided surgery, and biologic therapies aimed at modulating disease progression are set to revolutionize the landscape. These innovations could allow surgeons to intervene at a more precise window tailored to individual disease profiles, shifting the paradigm from reactive to proactive care. Personalized medicine, supported by genomic profiling and biomarker discovery, offers the potential to predict disease behavior more accurately and determine the optimal timing for intervention before irreversible nerve damage occurs. As these technologies mature, they promise to reduce complication rates and improve long-term outcomes, but also require careful integration into clinical workflows and ethical oversight.
If you are contemplating the timing of spine surgery or wish to explore personalized treatment options, consulting with a specialized spine surgeon is essential. Our expert team offers comprehensive evaluations and cutting-edge solutions tailored to your unique condition. Contact us today to schedule your consultation and take the first step toward optimized spinal health.
Harnessing Cutting-Edge Technologies to Predict Surgical Windows in Spinal Disorders
Emerging innovations such as machine learning algorithms and advanced neuroimaging techniques are revolutionizing how clinicians determine the optimal timing for spine surgery. By integrating big data analytics—drawing from patient-specific factors like genetic markers, biomechanical assessments, and symptom trajectories—surgeons can now forecast disease progression with unprecedented precision. For instance, studies published in the Journal of NeuroEngineering and Rehabilitation illustrate how predictive modeling can identify high-risk patients, enabling proactive intervention before irreversible nerve damage occurs.
Innovative Multidisciplinary Decision-Making: Beyond Conventional Criteria
The future of surgical timing lies in holistic, multidisciplinary frameworks that synthesize insights from neurology, orthopedics, psychology, and rehabilitation sciences. These collaborative approaches facilitate a comprehensive evaluation of neurological deficits, psychosocial factors, and patient lifestyle, fostering nuanced, patient-centered decisions. For example, incorporating mental health assessments ensures that psychological readiness complements physical health considerations, ultimately leading to better adherence and outcomes. Such integrative models are supported by recent guidelines from the American Association of Neurological Surgeons, emphasizing personalized care pathways.
What are the ethical considerations in opting for early versus delayed intervention in asymptomatic patients?
Deciding whether to proceed with prophylactic surgery in asymptomatic individuals with imaging anomalies remains ethically complex. The primary dilemma revolves around balancing the potential to prevent future disability against the risks of unnecessary surgical procedures. Ethical frameworks advocate for transparent shared decision-making, informed consent, and thorough risk-benefit discussions. Longitudinal cohort studies, such as those maintained by the National Spinal Cord Injury Statistical Center, provide critical data that inform these ethical debates, emphasizing the importance of evidence-based, patient-centered care.
Integrating Personalized Medicine to Tailor Surgical Timing Strategies
The advent of personalized medicine, supported by genomic profiling and biomarker discovery, promises to refine the timing of surgical interventions further. For instance, identifying genetic predispositions to rapid disease progression allows clinicians to intervene earlier in susceptible patients. Augmenting this approach, biologic therapies aimed at modulating inflammatory responses and neuroregeneration are under investigation, potentially extending the window for safe and effective surgery. As these therapies mature, they will enable a shift from reactive to proactive spinal care, reducing morbidity and improving long-term functional outcomes.
Visualizing the Future: The Role of Augmented Reality and 3D Printing in Surgical Planning
Augmented reality (AR) and 3D printing technologies are transforming preoperative planning, allowing surgeons to visualize complex spinal anatomy with remarkable clarity. These tools facilitate precise surgical interventions tailored to individual patient anatomy, enabling earlier and more confident operative decisions. For example, AR-guided surgery can highlight critical neural structures in real-time, reducing intraoperative risks and supporting earlier intervention strategies. The integration of these innovations promises to further refine the timing and safety of spinal surgeries.
Expert Insights & Advanced Considerations
1. Personalized Timing Strategies Enhance Outcomes
Tailoring surgical timing based on individual patient profiles, including genetic markers and disease progression patterns, leads to better recovery and reduced complications. Advanced diagnostic tools and predictive analytics enable clinicians to determine the precise window for intervention, emphasizing the importance of a customized approach in spinal care.
2. Integration of Multidisciplinary Data Improves Decision-Making
Combining insights from neurology, orthopedics, psychology, and rehabilitation sciences fosters a comprehensive assessment, ensuring that all relevant factors influence the timing of surgery. This multidisciplinary approach minimizes risks of overtreatment or delayed intervention, aligning with the latest evidence-based guidelines.
3. Emerging Technologies Are Transforming Surgical Planning
Innovations such as augmented reality (AR), 3D printing, and machine learning models are revolutionizing preoperative planning, allowing surgeons to visualize complex anatomy and disease trajectories more accurately. These tools support earlier and safer interventions, ultimately enhancing patient outcomes.
4. Ethical Frameworks Support Informed, Patient-Centered Decisions
Ethical considerations in deciding between early and delayed surgery emphasize informed consent, shared decision-making, and respecting patient preferences. Longitudinal data from studies like the National Spinal Cord Injury Statistical Center inform these complex choices, promoting transparency and trust.
5. Personalized Medicine Promises Future Precision in Surgical Timing
Genomic profiling and biomarker discovery are paving the way for highly individualized treatment plans. Identifying patients at high risk for rapid disease progression allows for proactive intervention, supported by biologic therapies that could extend the optimal window for surgery.
Curated Expert Resources
- Journal of Spinal Disorders & Techniques: Offers cutting-edge research and clinical guidelines on spinal surgery timing and techniques.
- American Association of Neurological Surgeons (AANS): Provides comprehensive guidelines and consensus statements on surgical decision-making.
- National Spinal Cord Injury Statistical Center: Supplies valuable longitudinal data informing ethical and clinical decisions.
- NeuroEngineering and Rehabilitation Journal: Features innovative studies on predictive analytics and machine learning applications in spine care.
- Advanced Spine Surgery Techniques (2025 Edition): A professional resource highlighting technological advancements impacting surgical timing.
Final Expert Perspective
Determining the optimal timing for spine surgery in NJ demands a sophisticated, patient-centered approach that integrates the latest technological innovations, multidisciplinary insights, and ethical considerations. As we advance toward personalized medicine, the ability to predict disease trajectories with precision will redefine surgical windows, translating into improved outcomes and quality of life. For those seeking expert guidance, engaging with a board-certified spine surgeon who stays abreast of these innovations is essential. Contact us today to explore personalized treatment strategies and stay at the forefront of spinal care.

