My Personal Encounter with Spine Surgery Dilemmas
As someone who has battled chronic back pain for years, I remember the day I finally decided to explore surgical options. The confusing array of choices, especially between disc resection and fusion surgery, left me overwhelmed. Sharing my journey, I hope to shed some light on these procedures based on my experience and research.
Understanding the Basics: What Are Disc Resection and Fusion Surgery?
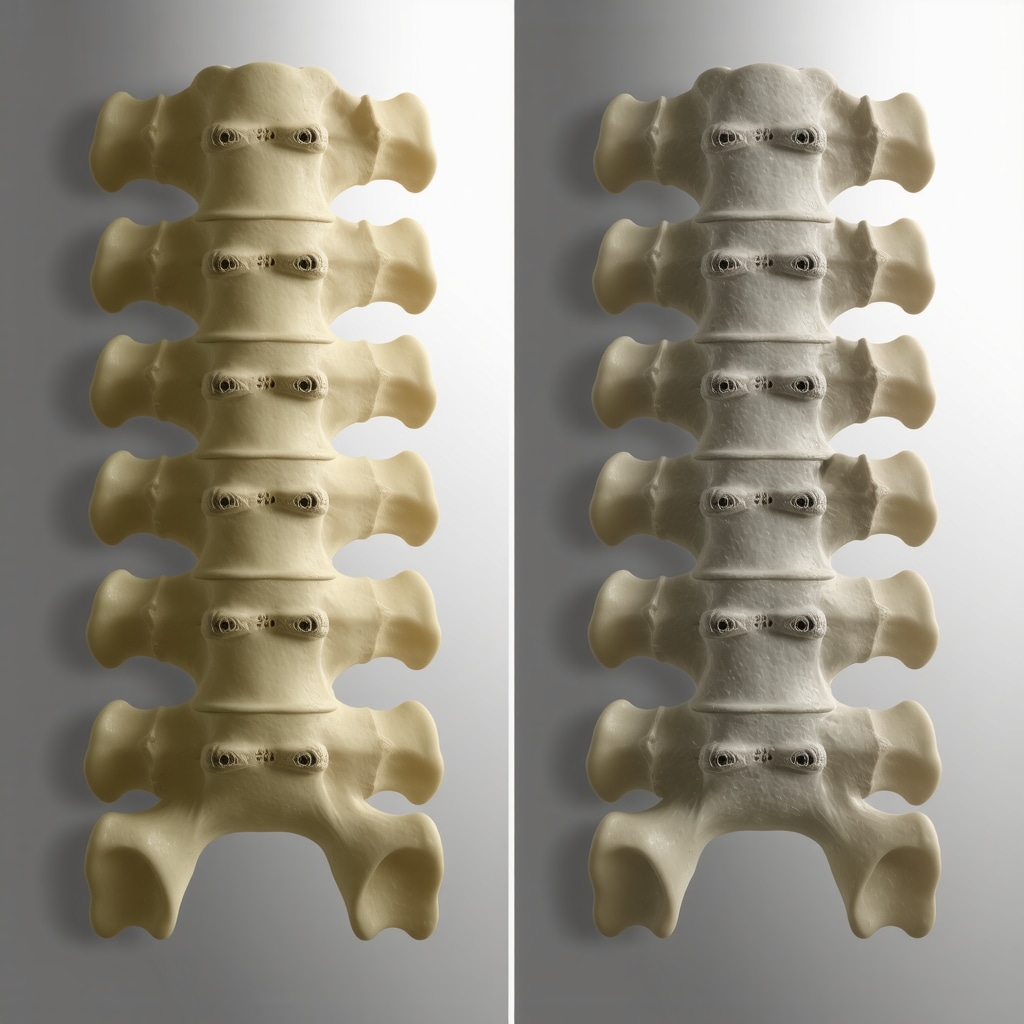
Disc resection, often known as discectomy, involves removing herniated or damaged disc material to relieve nerve pressure. Fusion surgery, on the other hand, permanently fuses two or more vertebrae to stabilize the spine. Both procedures aim to alleviate pain but differ significantly in approach and outcomes.
Weighing the Pros and Cons: Is One Better Than the Other?
What Are the Personal Benefits and Drawbacks of Disc Resection?
In my case, disc resection offered a less invasive option with a quicker recovery time. I appreciated that it preserved most of my spinal mobility. However, I was aware of the possibility of re-herniation, which could mean additional surgeries down the line. According to the American Academy of Orthopaedic Surgeons, discectomy is highly effective for herniated discs but may not be suitable for degenerative conditions requiring stabilization.
And What About Fusion Surgery? Is It a Long-Term Solution?
Fusion surgery provided a sense of long-term stability, especially in cases of spinal instability. My surgeon explained that fusing segments could help prevent future disc herniation at the same level. Nonetheless, I was cautious about the potential for reduced flexibility and the risk of adjacent segment disease, which studies suggest can occur over time (source).
Is Your Choice Based on Personal Goals and Lifestyle?
Deciding between these surgeries isn’t just about the technical differences; it’s about aligning with your personal health goals. For me, maintaining mobility was crucial, so disc resection made sense. If stability was more important, fusion might have been the right path. An important step I took was consulting with expert NJ spine surgeons, who guided me based on my condition and lifestyle.
How Do You Know Which Surgery Is Right for You?
It’s essential to have a thorough evaluation and discuss all options with a qualified specialist. I recommend exploring resources like this detailed guide to understand your specific case better.
If you’re considering spine surgery, I encourage you to share your experiences or ask questions in the comments below. Connecting with others who’ve faced similar decisions can provide invaluable support.
Deciphering the Complexities: Which Spinal Surgery Aligns with Your Lifestyle?
When facing a decision about spinal surgery, understanding the nuanced differences between procedures like disc resection and fusion surgery is crucial. For many patients, the choice hinges not only on medical necessity but also on personal goals, activity levels, and the potential impact on quality of life. An expert NJ spine surgeon emphasizes that personalized evaluation is paramount, considering factors such as degenerative changes, spinal stability, and future mobility requirements.
How Do Advanced Technologies Shape Surgical Outcomes?
Emerging innovations, including robotic-assisted techniques and minimally invasive approaches, are transforming the landscape. These advancements aim to reduce tissue trauma, improve precision, and accelerate recovery times. For example, robotic systems facilitate meticulous discectomy procedures, potentially lowering re-herniation risks. Similarly, minimally invasive fusion techniques, like lateral interbody fusion, are offering patients options with fewer complications and shorter hospital stays. Staying informed about these developments can help patients advocate for cutting-edge care and better outcomes.

What Are the Practical Implications of Long-Term Stability Versus Mobility?
One of the most critical considerations is how each surgical choice impacts long-term functionality. Fusion surgery, while providing stability—especially in cases of spinal instability—may lead to adjacent segment disease over time, necessitating further interventions. Conversely, disc resection preserves mobility but might require future procedures if re-herniation occurs. A comprehensive understanding of these trade-offs is essential; consulting with a board-certified NJ spine surgeon can help tailor decisions to individual lifestyles and expectations.
Are There Non-Surgical Alternatives That Could Delay or Prevent Surgery?
Before opting for invasive procedures, exploring non-surgical options such as advanced physical therapy, regenerative treatments, or epidural injections might be beneficial. Recent research highlights that such interventions can effectively manage symptoms and improve function in selected cases, possibly postponing or even avoiding surgery altogether (source). Understanding when these options are appropriate is a nuanced decision best made in collaboration with a spine specialist.
If you’re contemplating your surgical options, I invite you to share your questions or experiences in the comments below. Engaging with others who have navigated similar paths can provide valuable insights and support on your journey towards spine health.
What Deepens Your Understanding of Long-Term Outcomes in Spinal Surgery?
Reflecting on my personal journey and ongoing research, I’ve come to appreciate how each surgical approach impacts not just immediate relief but also the long-term quality of life. Fusion surgery’s promise of stability often comes with the caveat of adjacent segment degeneration, a phenomenon thoroughly documented by studies like those published in the Journal of Neurosurgery: Spine (source). Conversely, disc resection preserves mobility but raises questions about re-herniation risk over time. This nuanced understanding underscores the importance of personalized surgical planning, taking into account patient activity levels, age, and degenerative changes.
Balancing Innovation and Long-Term Outcomes in Spinal Surgery
In my ongoing exploration of spinal procedures, I’ve come to appreciate that the evolution of surgical techniques—particularly robotic-assisted and minimally invasive approaches—has profoundly shifted the landscape. These technological advances, like the robotic-assisted techniques, are not just about reducing recovery times but also about enhancing precision, which can significantly influence long-term stability and patient satisfaction. From my personal perspective, integrating these innovations requires discerning judgment, as not every case benefits equally. The key is understanding when a cutting-edge approach genuinely offers a tangible advantage over traditional methods, especially in complex cases involving degenerative disc disease or multi-level pathology.
Things I Wish I Knew Earlier (or You Might Find Surprising)
1. Not All Surgeries Are Created Equal
When I first faced the decision, I underestimated the importance of understanding the specific type of surgery. Disc resection and fusion surgery serve different purposes; one preserves mobility, while the other offers stability. Knowing which aligns with your lifestyle can make a world of difference.
2. The Power of a Good Surgeon
Choosing a highly experienced, board-certified NJ spine surgeon was crucial for my peace of mind. Their expertise directly impacted my recovery and long-term outcome. Don’t settle for less; your health deserves top-tier care.
3. Technology Can Be a Game-Changer
Emerging innovations like robotic-assisted surgery and minimally invasive techniques can significantly reduce recovery times and improve precision. If you’re exploring options, ask your surgeon about these advancements — they might be the key to better results.
4. Long-Term Outlook Matters
While immediate relief is vital, I’ve learned that understanding potential long-term effects, like adjacent segment disease after fusion, is equally important. A balanced approach considers both current needs and future well-being.
5. Non-Surgical Options Are Worth Considering
Sometimes, conservative treatments like physical therapy or regenerative medicine can delay or even prevent surgery. It’s worth exploring these before making irreversible decisions—your body may benefit from a less invasive path.
6. Personal Goals Should Drive the Decision
My choice was influenced by my desire to maintain mobility; others might prioritize long-term stability. Clearly defining what matters most to you will help guide your surgical options.
Resources I’ve Come to Trust Over Time
- American Academy of Orthopaedic Surgeons: Their comprehensive guides helped demystify surgical procedures and set realistic expectations. If you want reliable, evidence-based information, it’s a great place to start.
- Journal of Neurosurgery: Spine: For in-depth research on long-term outcomes like adjacent segment disease, this journal provides valuable insights that informed my understanding of risks and benefits.
- NJ Spine Surgeons Online: As a local resource, their articles and expert opinions are tailored to patients in New Jersey, making complex topics more accessible.
Parting Thoughts from My Perspective
Deciding between disc resection and fusion surgery is a deeply personal journey, shaped by your unique needs and goals. From my experience and research, I’ve realized that knowledge, technology, and expert guidance are your best allies. If this resonates with you, I’d love to hear your thoughts or experiences—sharing stories makes all of us better prepared for the road ahead. Remember, the right surgical choice can restore not just your back, but your confidence and quality of life. Feel free to explore more about your options and consult with qualified NJ spine surgeons to find your best path forward.