My Journey with Spine Pain: When I Started Questioning Surgery
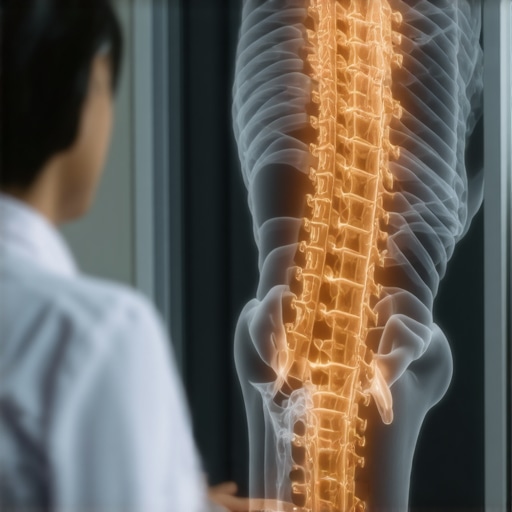
Like many others in New Jersey, I faced debilitating back pain that affected my daily life. Initially, I was eager to explore all options, including surgery. But as I researched, I found myself pondering: should I delay spine surgery? My experience taught me that timing and understanding the pros and cons are crucial before making such a significant decision.
The Hidden Benefits of Waiting: Gaining Perspective
One thing I realized early on is that delaying spine surgery can sometimes give you the chance to explore less invasive treatments. For example, I tried physical therapy and minimally invasive procedures that helped me avoid surgery altogether. According to experts, such approaches can be effective, especially if your condition isn’t urgent. For further insights, you might want to explore minimally invasive spine treatments to understand their benefits.
Risks of Waiting: When Delay Might Worsen Your Condition
However, I also learned that delaying surgery isn’t always advisable. If your condition progresses, it could lead to nerve damage or chronic pain. I remember reading that in cases of severe spinal stenosis or herniated discs, timely intervention can prevent long-term complications. The key is to consult with a trusted specialist who can assess your unique situation. For personalized advice, I recommend checking out signs you might need surgery.
Is It Better to Act Now or Wait? My Personal Reflection
Deciding whether to delay spine surgery is complex. In my case, I weighed the potential benefits of non-surgical options against the risk of condition worsening. I also considered the latest advancements, like robotic-assisted spine surgery, which may offer safer and more precise procedures if surgery becomes necessary.
How do I know if I’m delaying too long or acting too early?
This question haunted me during my decision-making process. The answer lies in thorough consultations with qualified surgeons who can evaluate your MRI scans and overall health. They can help you understand whether your symptoms warrant immediate surgery or if waiting could be beneficial. Remember, every case is unique, and expert guidance is essential.
If you’re grappling with similar questions, I encourage you to share your experience or ask for advice in the comments below. It’s comforting to know others are navigating the same path.
Ultimately, the decision to delay or proceed with spine surgery depends on individual circumstances, potential risks, and personal comfort levels. Being well-informed and consulting reputable specialists in NJ ensures you make the best choice for your health.
Understanding the Nuances of Timing in Spine Surgery Decisions
One of the most critical aspects of spine care is determining the optimal time for surgical intervention. As a seasoned spine specialist, I often see patients grappling with the dilemma: should I act now or wait? The answer isn’t straightforward and depends on multiple factors, including the severity of symptoms, progression of the condition, and individual health status. Recent advancements, such as innovative surgical techniques, are changing the landscape, making surgery safer and more effective when it becomes necessary.
Assessing the Impact of Delaying Surgery: Risks and Rewards
Delaying surgery might seem appealing, especially if your symptoms are manageable with conservative treatments like physical therapy or medication. However, this delay can sometimes lead to worsening nerve compression, increased pain, or even irreversible neurological damage. For instance, in cases of spinal stenosis, postponing surgery could result in diminished mobility and quality of life. A comprehensive evaluation by a qualified surgeon, often involving advanced imaging like MRI, can help you understand whether your condition warrants prompt action. To explore this further, consider reading about spinal decompression procedures in 2025.
What Are the Indicators That Signal It’s Time to Undergo Surgery?
Persistent symptoms such as unrelenting pain, weakness, numbness, or loss of bladder or bowel control are clear signs that surgery might be necessary. Additionally, radiological evidence showing nerve impingement or spinal instability can influence this decision. An essential step is consulting with a board-certified spine surgeon who can interpret your MRI and clinical signs accurately. For personalized guidance, many patients find it helpful to review signs indicating need for surgery.
How Future Technologies Are Reshaping Surgical Timing and Outcomes
Emerging technologies like robotic-assisted spine surgery and minimally invasive procedures are enabling surgeons to perform complex surgeries with less tissue damage and faster recovery times. These innovations are making the decision to operate less daunting and more precise, allowing for intervention at earlier stages when it can prevent long-term disability. Understanding these advancements can empower patients to make informed choices aligned with the latest standards of care.
Are there specific patient profiles that benefit most from early intervention versus delayed surgery?
This is a nuanced question. Generally, younger patients or those with progressive neurological deficits tend to benefit from earlier surgery, which can prevent irreversible damage. Conversely, older patients or those with comorbidities might opt for a cautious approach, balancing surgical risks against potential benefits. Consulting with specialists experienced in selecting a qualified surgeon in NJ ensures that individual factors are thoroughly evaluated, leading to tailored treatment plans.
If you’re contemplating your next step or unsure about the timing, I encourage you to share your questions or experiences in the comments. Connecting with others facing similar decisions can provide valuable perspective and reassurance.
Remember, the choice between immediate surgery and watchful waiting should always be made with expert guidance, considering your unique health circumstances and the latest technological advancements in spine surgery.
Balancing the Risks and Rewards of Early vs. Delayed Surgery: My Deep Dive
Reflecting on my journey, I realize that the decision to pursue spine surgery isn’t just about symptoms but also about understanding the nuanced risks and benefits involved. For example, emerging surgical techniques like the latest innovative procedures are transforming how we approach timing. These advancements allow for earlier interventions with less invasive options, which could potentially prevent irreversible nerve damage. Yet, I also learned that rushing into surgery without thorough evaluation might expose patients to unnecessary risks, especially if conservative treatments could suffice temporarily.
The Role of Advanced Technology in Shaping Surgical Timing
One of the most fascinating developments I encountered is robotic-assisted spine surgery. This technology offers incredible precision, reducing operative risks and improving recovery times. For patients like me, it opened the door to considering surgery at earlier stages, knowing that these innovations could significantly improve outcomes. Still, it’s essential to weigh the availability and suitability of such technology in your local area, which underscores the importance of consulting with experienced surgeons who are proficient in these cutting-edge techniques.
What Could Be the Consequences of Delaying Surgery Too Long?
From my experience, I understand that delays might seem appealing when symptoms are manageable, but there’s a fine line. According to expert insights, postponing surgery in cases of progressive nerve compression can lead to irreversible neurological deficits, which might diminish quality of life permanently. MRI scans and clinical evaluations are crucial to determine if your condition warrants immediate action. For those curious about how to assess their situation, I recommend reviewing the signs indicating when surgery is necessary.
When Is It Truly Time to Take the Surgical Leap?
In my case, persistent symptoms like weakness, unrelenting pain, and numbness eventually pushed me to seek surgical options. But beyond symptoms, radiological evidence such as nerve impingement or spinal instability played a pivotal role. Consulting with a board-certified spine surgeon helped me interpret these signs and make an informed decision. I encourage anyone facing this dilemma to consider comprehensive evaluations and personalized advice, as each case presents unique nuances that influence the optimal timing of intervention.
How Do Future Innovations Influence My Decision-Making?
The rapid evolution of spinal decompression techniques in 2025 and beyond has reshaped what I thought possible. These innovations mean that surgery can now be safer, less invasive, and more effective, even at earlier stages of disease progression. They also make me consider that waiting might sometimes result in missed opportunities for intervention when less invasive options could be highly effective. Staying informed about technological advances is essential for making decisions aligned with cutting-edge care.
What Advanced Questions Should Patients Ask Their Surgeons?
One question I found invaluable was: “Are there particular patient profiles that benefit most from early intervention versus delayed surgery?” The answer often depends on age, progression rate, and neurological impact. For example, younger patients or those exhibiting rapid deterioration might gain the most from prompt surgery, while older individuals or those with comorbidities might prioritize conservative management longer. To find a surgeon adept at tailoring these decisions, I suggest exploring tips for selecting a top NJ spine surgeon. If you’re navigating these choices, I invite you to share your experiences or questions in the comments—sometimes, learning from others’ journeys offers invaluable perspective.
Ultimately, the timing of spine surgery is a complex interplay of clinical signs, technological options, and personal comfort. Staying informed and engaging with experienced specialists ensures you make choices that serve your long-term health and well-being.
The Subtle Art of Surgical Timing: When Innovation Meets Patient Needs
Deciding on the optimal moment for spine surgery often feels like navigating a complex labyrinth. While traditional indicators such as persistent neurological deficits or radiological evidence guide many, recent technological advancements are reshaping the landscape. For instance, the latest in spinal decompression techniques in 2025 emphasize early intervention, especially when emerging minimally invasive options promise less tissue damage and faster recovery. As a seasoned clinician, I’ve observed that integrating these innovations into decision-making frameworks allows for more nuanced, individualized care plans, ultimately enhancing patient outcomes.
The Risks of Relying Solely on Traditional Timelines
While waiting might seem prudent, especially when conservative therapies provide relief, I’ve encountered cases where delays resulted in irreversible neurological impairments. The danger lies in underestimating the insidious progression of nerve compression, which can silently lead to diminished function. According to recent evidence, such as the comprehensive review in Risks and benefits of spinal fusion in NJ, timely surgical intervention can prevent long-term disabilities, reinforcing the importance of early, expert assessment.
Can Future Technologies Truly Revolutionize Surgical Decisions?
Absolutely. Innovations like robotic-assisted spine surgery are not mere fads but transformative tools that enhance precision and safety, making earlier intervention more feasible. These technologies also facilitate complex procedures with minimal invasiveness, which previously might have been deferred due to surgical risk concerns. My personal experience with such advancements has shown that they empower patients and surgeons alike to explore earlier surgical options without compromising safety, especially relevant for younger individuals or those with progressive symptoms.
How can patients and clinicians collaborate to optimize surgical timing using these innovations?
Open dialogue is critical. Patients should feel encouraged to seek comprehensive evaluations that incorporate these technologies, asking their surgeons about the latest in decompression procedures and robotic techniques. Likewise, clinicians must stay abreast of emerging evidence and integrate advanced diagnostics into their practice. Engaging in shared decision-making ensures that the chosen timing aligns with individual disease progression, technological availability, and personal preferences, ultimately leading to tailored, effective treatment strategies.
If you’re contemplating whether to act now or wait, consider consulting specialized centers that utilize these cutting-edge tools. Your proactive approach, combined with expert guidance, can significantly alter your trajectory toward recovery and long-term wellness. For further insights, I invite you to explore my detailed discussions on modern decompression techniques and robotic-assisted surgeries, designed to empower informed choices and optimal outcomes.
Things I Wish I Knew Earlier (or You Might Find Surprising)
The Power of Patience
One of the most unexpected lessons in my spine journey was realizing that sometimes, waiting and exploring less invasive treatments can lead to surprisingly good outcomes. I initially thought surgery was my only option, but physical therapy and newer techniques showed me the value of patience and cautious optimism.
The Hidden Dangers of Delay
I learned firsthand that delaying surgery isn’t always harmless. When symptoms worsen or nerve compression becomes severe, the risk of irreversible damage increases. My experience taught me to recognize the importance of timely intervention, guided by expert advice.
Technology as a Game-Changer
Advancements like robotic-assisted surgery and minimally invasive techniques are reshaping how we approach timing. These innovations sometimes allow for earlier intervention with less risk, changing the traditional wait-and-see approach.
Listening to Your Body and Experts
Ultimately, my journey reinforced that paying close attention to persistent symptoms and consulting experienced specialists is crucial. Every case is unique, and personalized advice makes all the difference.
Resources I’ve Come to Trust Over Time
- National Spine Health Foundation: Their evidence-based resources helped clarify my options and risks, making complex decisions easier.
- American Academy of Orthopaedic Surgeons: Trusted for their comprehensive guides on spine conditions and surgical innovations.
- SpineUniverse: A user-friendly platform with expert articles that deepen understanding of procedures like spinal decompression.
- Journal of Neurosurgery: For those who want to delve into the latest research and technological advances in spine surgery.
Parting Thoughts from My Perspective
Deciding when to undergo spine surgery is deeply personal and complex. From my experience, understanding the latest innovations and listening carefully to your body and medical team can lead to better, more informed choices. Remember, there’s no one-size-fits-all answer—what matters most is finding a path that aligns with your health and comfort levels. If this resonates with you, I’d love to hear your story or thoughts. Sharing our experiences can make this journey less daunting for everyone.
,