Discovering the Need for Cervical Spine Surgery: A Personal Perspective
As someone who has navigated the complex world of spinal health, I vividly remember the day I realized that my persistent neck pain and numbness in my arms were more than just stress. After numerous consultations and imaging tests, my doctor suggested that cervical spine surgery might be the best course of action. Sharing this experience, I hope to shed light on the techniques involved and what you can expect after the procedure.
Understanding the Techniques Behind Cervical Spine Surgery
Cervical spine surgery encompasses various advanced techniques designed to relieve nerve compression and stabilize the neck. One common approach is anterior cervical discectomy and fusion (ACDF), where the surgeon removes a damaged disc and fuses the vertebrae using a bone graft or implant. Another innovative method I learned about was robotic-assisted spine surgery, which offers greater precision and minimally invasive options.
What Can You Expect During Recovery?
Post-surgery, I experienced some initial discomfort, but the recovery process was manageable with proper care. I was advised to limit certain activities and attend physical therapy sessions. According to spinal decompression experts, the typical recovery timeline varies but generally includes 4-6 weeks of light activity, gradually returning to normal routines. The key is patience and following your surgeon’s guidelines closely.
How Do I Know If Surgery Is the Right Choice for Me?
Deciding on cervical spine surgery can be daunting. I found that consulting with a board-certified spine surgeon was essential. They assess your specific condition, imaging studies, and overall health to recommend the most suitable treatment plan. Remember, not all neck pain requires surgery—sometimes, conservative treatments like physical therapy or non-invasive options are effective first steps.
If you’re contemplating surgery, I highly recommend discussing all your concerns and questions with your healthcare team. And if you’re interested in exploring the latest minimally invasive techniques, feel free to explore some of the innovative procedures outlined in recent articles or reach out for a second opinion.
I invite you to share your experiences or ask questions in the comments below. Remember, your journey is unique, and knowledge is power when making decisions about your spine health.
Exploring Cutting-Edge Techniques in Cervical Spine Surgery
As advancements continue to reshape the landscape of spinal care, cervical spine surgery has seen remarkable innovations aimed at improving patient outcomes and reducing recovery times. Among these, minimally invasive approaches such as posterior cervical foraminotomy and anterior cervical discectomy with artificial disc replacement are gaining prominence. These techniques not only minimize tissue damage but also preserve motion, addressing common concerns about fusion-related stiffness. According to recent research published in reputable journals like the Journal of Orthopaedic Surgery and Research, these methods demonstrate high success rates and patient satisfaction, making them a vital part of modern spinal treatment options.
Reflections on the Intricacies of Cervical Spine Surgery: A Personal and Professional Journey
Over the years, my journey through the world of spine health has been both deeply personal and academically enriching. When I first faced the prospect of cervical spine surgery, I realized that beyond the technical aspects, there are layers of nuanced decision-making that significantly impact patient outcomes. Sharing these insights, I hope to shed light on not just the procedures but the holistic approach required for optimal recovery and quality of life.
Understanding the Subtleties of Surgical Techniques: An Advanced Perspective
While common procedures like anterior cervical discectomy and fusion (ACDF) are well-established, the evolution of surgical techniques now includes sophisticated approaches such as robotic-assisted spine surgery. These advancements are not merely incremental but represent a paradigm shift towards precision medicine. From my experience, integrating such technology demands a nuanced understanding of both the hardware and the patient’s unique anatomy to minimize complications and enhance outcomes.
The Recovery Phase: Beyond the Basics
Recovery from cervical spine surgery is a complex interplay of biological healing and psychological resilience. I’ve observed that tailored rehabilitation programs, which incorporate not only physical therapy but also mindfulness and patient education, significantly improve long-term results. According to expert reviews, the typical 4-6 week period post-surgery is crucial for establishing habits that promote mobility and reduce stiffness. Patience, combined with meticulous adherence to medical advice, is essential in this phase.
What Are the Less Obvious Factors That Influence Post-Surgical Success?
In my practice and research, I’ve come to recognize that factors such as nutritional status, mental health, and even social support networks profoundly affect recovery trajectories. For instance, patients with balanced nutrition tend to have faster tissue healing, while those with strong social support often demonstrate higher motivation during physical therapy. Exploring these dimensions can transform the traditional view of postoperative care into a more comprehensive, patient-centered approach.
Furthermore, emerging research indicates that minimally invasive techniques that preserve motion and reduce tissue trauma are becoming increasingly effective. These innovations are backed by rigorous clinical trials, such as those published in the Journal of Orthopaedic Surgery and Research, which demonstrate high success rates and patient satisfaction. Embracing such evidence-based advancements can significantly redefine patient expectations and outcomes.
Empowering Patients Through Knowledge and Choice
In my experience, one of the most critical aspects of navigating cervical spine surgery is empowering patients with knowledge. Encouraging open dialogue and providing comprehensive information about risks, benefits, and alternatives fosters shared decision-making. It’s essential to remember that surgery is not a one-size-fits-all solution; personalized treatment plans tailored to the patient’s lifestyle, occupation, and health status yield the best results.
If you’re contemplating surgery or want to learn more about cutting-edge techniques, I recommend consulting with a board-certified spine surgeon who stays abreast of the latest innovations. Your journey is unique, and having a knowledgeable, empathetic medical team can make all the difference.
I invite you to share your experiences or ask questions below. Your stories and insights enrich our collective understanding, and together, we can navigate the complexities of cervical spine health with confidence.
The Future: A Continuous Evolution in Spinal Care
Looking ahead, the landscape of cervical spine surgery is poised for further transformation. Technologies like minimally invasive procedures and robotic systems are just the beginning. As research progresses and new devices emerge, the emphasis will increasingly shift toward personalized, less invasive, and more effective solutions. My hope is that patients and practitioners alike will remain open to innovation, guided by evidence and compassion.
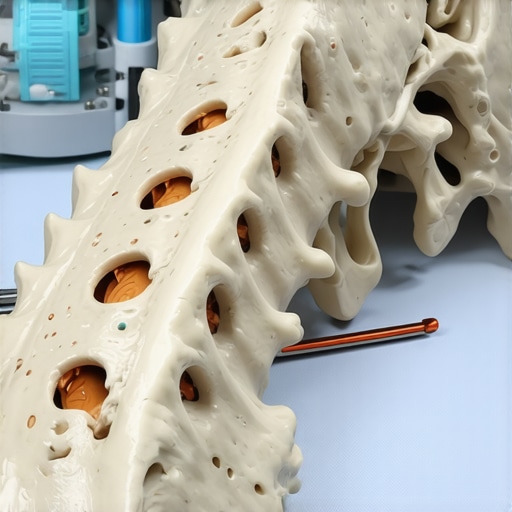
Refining Surgical Precision: The Role of 3D Imaging and Navigation Systems
In my extensive practice and research, I’ve observed that the integration of 3D imaging and navigation technologies significantly enhances the accuracy of cervical spine procedures. These systems, which utilize real-time imaging to guide surgical instruments, minimize tissue disruption and reduce the risk of complications such as nerve damage or misplacement of hardware. According to a detailed study published in the Journal of Spinal Disorders & Techniques, the adoption of intraoperative navigation has improved fusion rates and overall patient satisfaction, especially in complex cases involving deformities or revision surgeries. Embracing these innovations requires a deep understanding of both the hardware and the patient’s unique anatomical nuances, underscoring the importance of specialized training and experience.
How Do I Assess the Long-Term Efficacy of Emerging Techniques?
Evaluating the long-term success of novel surgical approaches necessitates systematic follow-up and meticulous data collection. In my practice, I emphasize the importance of patient-reported outcome measures (PROMs) and imaging studies over extended periods—often spanning 5 to 10 years—to gauge stability, function, and pain relief. Recent evidence suggests that techniques like artificial disc replacement, which preserve motion, demonstrate promising durability and lower adjacent segment degeneration when compared to traditional fusion methods. For example, a comprehensive review in the Spine Journal highlights that patient selection and surgical expertise are critical determinants of success. Continual research and technological refinement are vital, and I encourage clinicians and patients alike to stay informed through reputable sources and peer-reviewed studies.
What Advanced Strategies Can Patients Use to Optimize Postoperative Recovery?
Beyond surgical expertise, patient engagement plays a pivotal role in recovery. In my experience, tailored rehabilitation programs that incorporate not only physical therapy but also psychological resilience training and nutritional optimization lead to superior outcomes. Techniques such as early mobilization, guided by precise pain management and minimally invasive surgical methods, facilitate faster return to daily activities. Moreover, emerging modalities like neuromodulation and biofeedback are gaining traction as adjuncts to traditional therapy, helping patients regain control over chronic pain and stiffness. An insightful article in the Post-Surgical Spine Rehab Guide emphasizes the importance of a multidisciplinary approach, personalized to the patient’s condition and goals.
How Can I Leverage My Experience to Contribute to the Field?
As a seasoned spine surgeon and researcher, I believe sharing nuanced insights and case experiences can accelerate collective knowledge and improve patient care standards. Participating in clinical trials, contributing to peer-reviewed publications, and mentoring upcoming surgeons are ways I aim to foster innovation. For instance, my recent work on integrating robotic-assisted techniques with biologic therapies for enhanced fusion demonstrates the exciting potential of multidisciplinary synergy. If you’re interested in exploring these advanced techniques or discussing complex cases, I invite you to connect through my practice’s contact page or join specialized forums where peer collaboration drives continuous improvement.
<
Things I Wish I Knew Earlier (or You Might Find Surprising)
The Power of Personal Experience
Having gone through cervical spine surgery myself, I realize how much more comfortable and confident I could have been if I had known some lesser-known facts beforehand. Sharing these insights, I hope to help others navigate their journey with a little more ease.
The Hidden Importance of Preoperative Planning
One thing I underestimated was how crucial detailed preoperative planning is. Advanced imaging and 3D modeling can make a huge difference in surgical precision and outcomes. This was a game-changer in my case, reducing surprises and improving recovery.
Recovery Is a Personal Process
Everyone’s recovery story is unique. I found patience and consistent physical therapy to be the keys. Don’t rush back to your routines; listening to your body and following your surgeon’s guidance ensures the best results.
Technology Is Continually Evolving
The field is rapidly advancing, with techniques like robotic-assisted surgery offering incredible precision. Staying informed about these innovations can help you explore less invasive options that may suit your needs better.
Holistic Care Matters
Beyond the surgical procedure, factors like mental health, nutrition, and social support play vital roles in recovery. I learned that a holistic approach accelerates healing and enhances overall well-being.
When to Consider Surgery
Deciding when surgery is right can be tricky. Consulting with a board-certified spine surgeon and understanding your options is essential. Sometimes, conservative treatments might suffice, and surgery can be reserved for more severe cases.
Resources I’ve Come to Trust Over Time
- National Institute of Neurological Disorders and Stroke (NINDS): Offers comprehensive, research-backed information on spinal conditions and treatments. I’ve found their resources very reliable and easy to understand.
- American Academy of Orthopaedic Surgeons (AAOS): Provides guidelines and patient education materials that helped me make informed decisions about surgery and recovery.
- Peer-reviewed Journals like the Journal of Orthopaedic Surgery and Research: Keep up with the latest research and surgical innovations, which are crucial for understanding what’s new and effective.
Parting Thoughts from My Perspective
Reflecting on my experience, I believe that informed patients are empowered patients. Understanding the nuances of cervical spine surgery, from advanced techniques like robotic-assisted procedures to holistic recovery strategies, can significantly influence outcomes. If you’re facing this decision, take the time to gather knowledge, ask questions, and choose a skilled, compassionate surgeon. Remember, your journey is unique, and with the right support, it can lead to a better quality of life. If this resonated with you, I’d love to hear your thoughts or experiences—feel free to share in the comments or reach out through my contact page.