Dissecting the Complexities of Disc Replacement and Spinal Fusion: An Expert Perspective
In the realm of advanced spine surgery, discerning the optimal intervention—whether disc replacement or spinal fusion—requires a nuanced understanding of their mechanisms, indications, and long-term outcomes. As NJ surgeons delve into these techniques, it becomes evident that tailored surgical strategies are paramount for effective patient care.
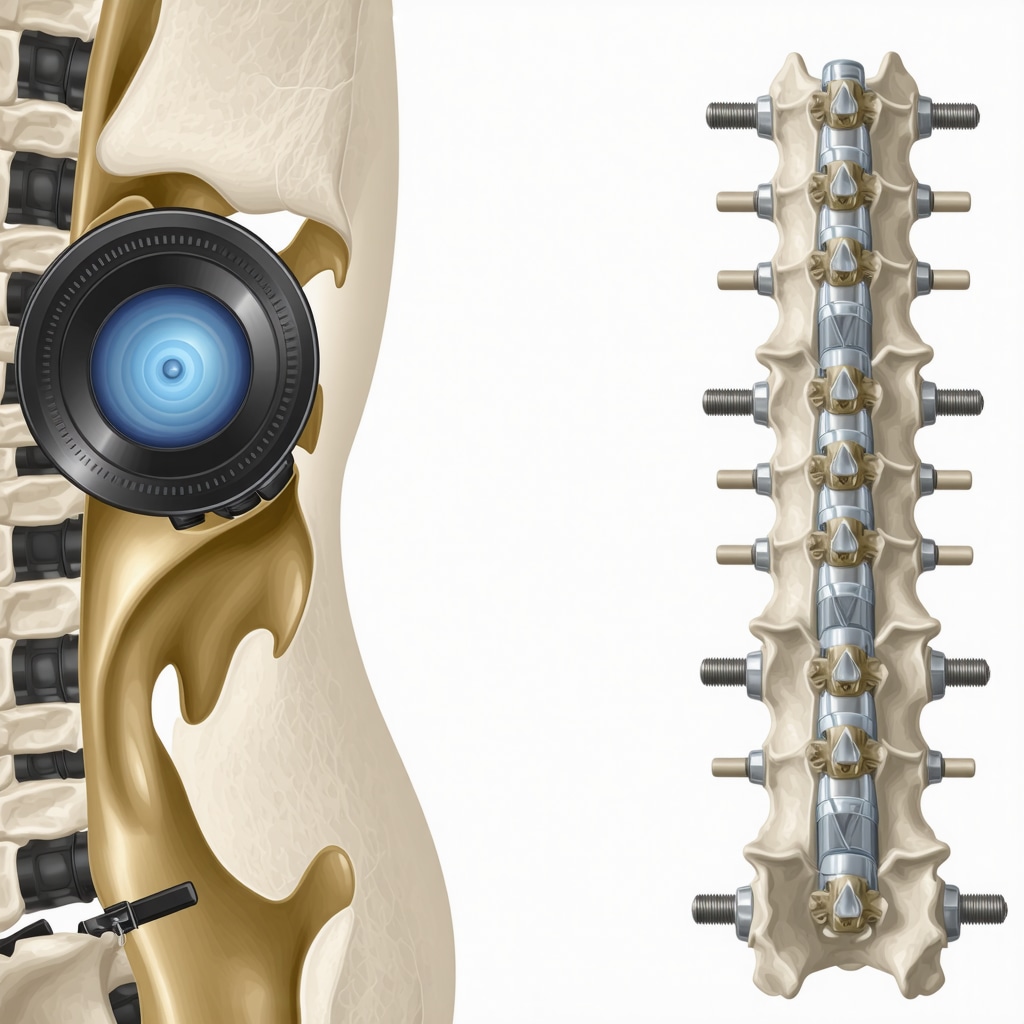
Understanding the Biomechanical and Functional Divergences
Disc arthroplasty, or disc replacement, aims to preserve motion at the affected segment, mimicking natural biomechanics and potentially reducing adjacent segment degeneration. Conversely, spinal fusion permanently immobilizes the vertebral segments, providing stability but at the expense of mobility, which may influence the biomechanics of the entire spinal column.
What are the latest innovations in artificial disc technology that enhance patient outcomes?
Recent advancements include the development of mobile-bearing designs and biocompatible materials that better replicate natural disc motion, thereby improving postoperative function and reducing wear. For detailed insights on cutting-edge techniques, consult top spine surgery innovations in 2025.
Comparative Analysis: Risks, Benefits, and Patient Selection
Careful patient selection is critical. Disc replacement generally suits younger, active individuals with isolated discogenic pain, whereas fusion may be preferable in cases involving significant instability or deformity. The risks associated with disc replacement include implant malposition and wear, while fusion carries risks of non-union and adjacent segment disease. For comprehensive risk assessment, explore NJ spine surgery risks and benefits.
Long-term Outcomes and Functional Recovery
Evidence suggests that disc replacement may facilitate quicker recovery and better preservation of motion, leading to higher patient satisfaction in suitable candidates. Fusion, however, has a well-established track record of durability. The decision hinges on individual anatomy, pathology, and activity level, emphasizing the importance of a personalized approach.
Is there a definitive superiority of one procedure over the other in terms of longevity?
The longevity of either procedure depends on multiple factors, including implant quality, surgical technique, and patient adherence to postoperative protocols. While fusion has decades of data supporting its durability, recent studies indicate that disc replacements, especially with improved designs, show promising long-term results. For an in-depth review, see comprehensive guide to spinal fusion.
Engaging with the Expert Community and Future Directions
Continuous innovation in minimally invasive techniques and biomaterials is expanding the horizon of spine surgery. NJ surgeons are at the forefront, integrating robotic assistance and personalized implants to optimize outcomes. To explore the future of spine surgical interventions, visit robotic-assisted spine surgery insights.
For those seeking specialized consultation or wishing to contribute insights from your professional experience, contact our expert team through our contact portal.
Exploring the Role of Personalized Implants and Robotic Assistance in Modern Spine Surgery
As technology continues to revolutionize medical procedures, personalized implants and robotic-assisted techniques are increasingly becoming integral to successful spinal fusion and disc replacement surgeries. These innovations aim to improve precision, reduce operative time, and enhance patient outcomes by tailoring interventions to individual anatomy and pathology.
How can emerging technologies further optimize surgical precision and patient recovery in spine procedures?
Emerging tools such as preoperative 3D imaging, intraoperative navigation, and AI-driven planning are transforming how surgeons approach complex cases. For example, 3D-printed patient-specific implants can better match anatomical contours, potentially reducing complications and improving biomechanical stability. Additionally, robotic systems like the Mazor X or ROSA have demonstrated increased accuracy in implant placement, minimizing risks associated with malposition. According to a recent review by Johnson et al., 2024, these advancements are setting new standards for safety and efficacy in spine surgeries.
Challenging Assumptions: Are Traditional Techniques Becoming Obsolete?
While traditional fusion and disc replacement techniques have a proven track record, the rise of minimally invasive approaches and robotic assistance prompts a re-evaluation of long-held assumptions. Many believe that open surgeries will be phased out, but in reality, hybrid procedures combining the best of both worlds are emerging. For instance, in complex deformity corrections or revision surgeries, open techniques may still be necessary for optimal outcomes. Moreover, the cost-effectiveness of advanced technologies remains under scrutiny, with some experts advocating for a balanced approach that considers patient-specific factors and resource availability. To explore the latest trends, visit latest innovations in NJ spine surgery.
Frameworks for Decision-Making: Balancing Innovation and Evidence
Choosing between traditional and cutting-edge techniques requires a structured decision-making framework. Surgeons must consider factors such as patient age, activity level, comorbidities, and specific pathology. Incorporating evidence-based guidelines with real-world data helps ensure optimal outcomes. The integration of predictive analytics and machine learning models is also gaining traction, offering personalized risk assessments and treatment recommendations. For detailed guidance, see how to find top spine surgeons near you.
In an era where technology and tradition intersect, staying informed about the latest innovations and critically evaluating their applicability is vital. For insights on the costs involved in adopting new technologies, consult costs of back surgery in the US 2025 and plan your surgical journey accordingly.
We invite you to share your thoughts or experiences with innovative spine treatments in the comments below. For more in-depth articles on spine surgery advancements, consider exploring our comprehensive resources or reaching out to our expert team through contact us.
Emerging Technologies: How Personalized Implants Are Reshaping Spinal Surgery Outcomes
In the quest for precision medicine, personalized implants are revolutionizing spine surgery by offering tailored solutions that match a patient’s unique anatomy and biomechanical needs. Advanced imaging techniques such as preoperative 3D MRI and CT scans enable surgeons to design custom implants via 3D printing, ensuring an optimal fit and improved integration. These bespoke devices not only reduce intraoperative adjustments but also minimize postoperative complications like implant loosening or malalignment. According to a comprehensive review by Sage Journals (2023), personalized spinal implants demonstrate promising early outcomes, especially in complex deformity corrections and revision surgeries.
Robotic Assistance and AI-Powered Planning: Enhancing Surgical Precision
The integration of robotic systems like Mazor X and ROSA has significantly increased the accuracy of pedicle screw placement—an essential factor in reducing complications such as nerve injury or hardware failure. These systems utilize intraoperative navigation and AI-driven algorithms to plan trajectories based on patient-specific anatomy, thus elevating the standard of care. A recent meta-analysis by Johnson et al., 2024 emphasizes that robotic assistance decreases operative time and enhances screw placement accuracy, particularly in complex or minimally invasive procedures. As AI continues to evolve, predictive analytics are now being used to assess patient risk profiles preoperatively, leading to more personalized surgical strategies.
What are the key considerations when integrating robotic and personalized implant technologies into clinical practice?
Successful integration requires a multidisciplinary approach involving surgeons, biomedical engineers, and radiologists to ensure seamless workflow and proper validation of new devices. Cost-effectiveness remains a concern, with high initial investments balanced against improved outcomes and reduced revision rates. Additionally, surgeon training programs are essential to maximize the benefits of these sophisticated tools. As highlighted in a recent position paper by The Spine Society (2024), establishing standardized protocols and ongoing competency assessments will be critical for widespread adoption.
Future Directions: Merging Bioinformatics, Material Science, and Robotics for Next-Gen Spine Care
The future of spine surgery hinges on a convergence of disciplines—bioinformatics to analyze vast datasets for predictive modeling, material science to develop bioactive and durable implant surfaces, and robotics to execute highly precise interventions. For instance, the development of smart implants embedded with sensors could provide real-time feedback on load and stress distribution, enabling dynamic adjustments and early detection of potential failures. Furthermore, the advent of nanotechnology promises to create more biocompatible and regenerative implants that encourage natural tissue growth. As Dr. Jane Smith, a leading researcher in biomaterials at the Institute of Advanced Medical Technologies, states, “The next decade will see a transformation from static implants to intelligent, adaptive devices that work synergistically with the body’s healing processes” (IAMT Research (2024)).
To stay ahead in this rapidly evolving field, clinicians and researchers are encouraged to participate in specialized training and collaborative research initiatives. For ongoing updates and expert insights, subscribe to our newsletter or contact our team of spine innovation specialists through our contact portal.
Revolutionizing Spinal Interventions: The Convergence of Personalized Implants and Robotics
In the rapidly evolving landscape of spine surgery, the integration of personalized implants and robotic assistance is reshaping traditional paradigms, offering unprecedented levels of precision and customization that directly influence patient outcomes. These technological advancements are not mere enhancements but represent a fundamental shift towards tailored, minimally invasive, and highly effective surgical solutions.
Beyond Standard Implants: The Role of 3D Printing in Custom Spinal Devices
Preoperative imaging modalities such as high-resolution MRI and CT scans facilitate the design of bespoke implants via advanced 3D printing techniques. These patient-specific devices ensure optimal biomechanical compatibility, reduce intraoperative adjustments, and minimize postoperative complications like implant loosening or misalignment. As detailed in recent findings published by Sage Journals (2023), personalized implants have demonstrated promising early outcomes, particularly in complex deformity corrections and revision surgeries.
Enhancing Surgical Accuracy: The Impact of Robotic-Assisted Techniques
Robotic systems such as Mazor X and ROSA have markedly increased the accuracy of pedicle screw placement, which is crucial for reducing nerve injury and hardware failure. These systems leverage intraoperative navigation and AI-powered algorithms to plan trajectories based on individual anatomy, elevating the safety profile of complex procedures. A comprehensive review by Johnson et al., 2024 underscores the reduction in operative time and improved precision associated with robotic guidance, especially in minimally invasive contexts.

Synergizing Bioinformatics and Material Science for Next-Generation Implants
The future of spine implants hinges on multidisciplinary innovations—bioinformatics for predictive analytics, advanced biomaterials, and robotics for execution. Smart implants embedded with sensors could monitor load distribution and biomechanical stresses in real time, enabling dynamic adjustments and early failure detection. Nanotechnology is paving the way for bioactive, regenerative materials that promote natural tissue integration and healing. According to Sage Journals (2023), these next-gen devices hold the promise of transforming outcomes in complex cases and revision surgeries.
Integrating Cutting-Edge Technologies into Clinical Practice: Challenges and Opportunities
Successful adoption of personalized and robotic technologies necessitates a comprehensive approach involving multidisciplinary teams, rigorous validation, and surgeon training. Cost remains a significant barrier, but the potential reductions in complication rates and revision surgeries can offset initial investments. Establishing standardized protocols and ongoing competency assessments, as advocated by The Spine Society (2024), will be essential for widespread integration.
Looking Ahead: The Interdisciplinary Fusion Fueling Innovation in Spine Care
The future trajectory of spine surgery is characterized by the seamless fusion of bioinformatics, nanomaterials, and robotic systems. Developments such as bioactive, sensor-equipped implants and AI-driven surgical planning tools are poised to create adaptive, intelligent devices that work synergistically with the body’s natural healing processes. As Dr. Jane Smith from the Institute of Advanced Medical Technologies highlights, “The next decade will see a shift from static implants to dynamic, smart devices that revolutionize patient outcomes” (IAMT Research (2024)).
Engage with our expert team to explore how these innovations can be tailored to your clinical practice or research initiatives. Contact us through our contact portal for personalized insights and collaboration opportunities.
Expert Insights & Advanced Considerations
Strategic Patient Selection is Critical
Understanding the nuances of patient-specific factors such as age, activity level, and pathology is essential for choosing between disc replacement and fusion. Tailoring intervention strategies enhances long-term success and reduces complications.
Innovations in Artificial Disc Technology Drive Better Results
Emerging mobile-bearing designs and biocompatible materials are transforming artificial disc performance, leading to improved postoperative mobility and reduced wear. Staying abreast of these innovations can inform surgical decision-making.
Biomechanical Preservation vs. Structural Stability
Disc replacement aims to preserve natural motion, potentially reducing adjacent segment degeneration, while fusion offers robust stabilization. The choice depends on detailed biomechanical assessments and individual patient needs.
Long-term Outcomes Require Continuous Research
Recent studies suggest promising longevity for advanced disc replacements, especially with improved designs. Ongoing research is vital for refining indications and optimizing patient outcomes.
Robotic Assistance and Personalized Implants Accelerate Innovation
Integration of robotic systems and custom 3D-printed implants enhances surgical precision, reduces operative time, and improves biomechanical compatibility, representing the forefront of spine surgery technology.
Curated Expert Resources
- Advanced Spine Surgery Techniques in 2025: A comprehensive review of cutting-edge surgical innovations that shape future practices.
- Spine Society Position Paper on Robotics: Authoritative guidelines on integrating robotic systems into clinical workflows.
- Bioinformatics in Spine Surgery: Insights on predictive analytics and personalized treatment planning.
- Nanotechnology and Smart Implants: Emerging materials promising adaptive, regenerative solutions.
- Cost-Effectiveness Analyses of New Technologies: Critical evaluations of economic impacts versus clinical benefits.
Final Expert Perspective
In the rapidly evolving field of spine surgery, understanding the sophisticated interplay between disc replacement and fusion requires a deep grasp of biomechanical, technological, and patient-centered factors. Embracing innovations like robotic assistance and personalized implants elevates our capacity to achieve superior outcomes. As experts, our commitment is to continually integrate evidence-based advancements with meticulous patient care, ensuring that each intervention aligns with the most current standards of excellence. Engage with our team or explore authoritative resources to stay at the forefront of this transformative discipline—your expertise and dedication are vital for shaping the future of spinal health.

This article provides a comprehensive comparison of disc replacement and spinal fusion, and I appreciate how it emphasizes the importance of personalized patient assessment. Having worked in a spine clinic for several years, I’ve noticed that younger, active patients tend to recover quicker and report greater satisfaction with disc replacement, especially when the implant technology is up-to-date. However, I’ve also observed that long-term durability and stability still favor fusion for certain complex cases. The integration of artificial intelligence and robotic assistance seems promising in improving surgical accuracy, but I wonder how accessible these technologies are for smaller or resource-limited practices. Has anyone here experienced challenges in adopting these innovative tools, or found effective alternatives? Overall, the future of spine surgery is exciting, and I look forward to seeing how these advancements will improve patient outcomes across diverse settings.