Strategic Considerations in Choosing Between Disc Resection and Fusion Surgery
In the evolving landscape of spinal surgery, discerning the optimal intervention for degenerative disc disease or herniation remains a critical challenge. Two prominent surgical modalities—disc resection and spinal fusion—offer distinct biomechanical and clinical outcomes. Expert spine surgeons in New Jersey emphasize a tailored approach, integrating patient-specific anatomical, functional, and lifestyle factors to maximize efficacy and minimize long-term morbidity.
Biomechanical Implications and Clinical Outcomes of Disc Resection
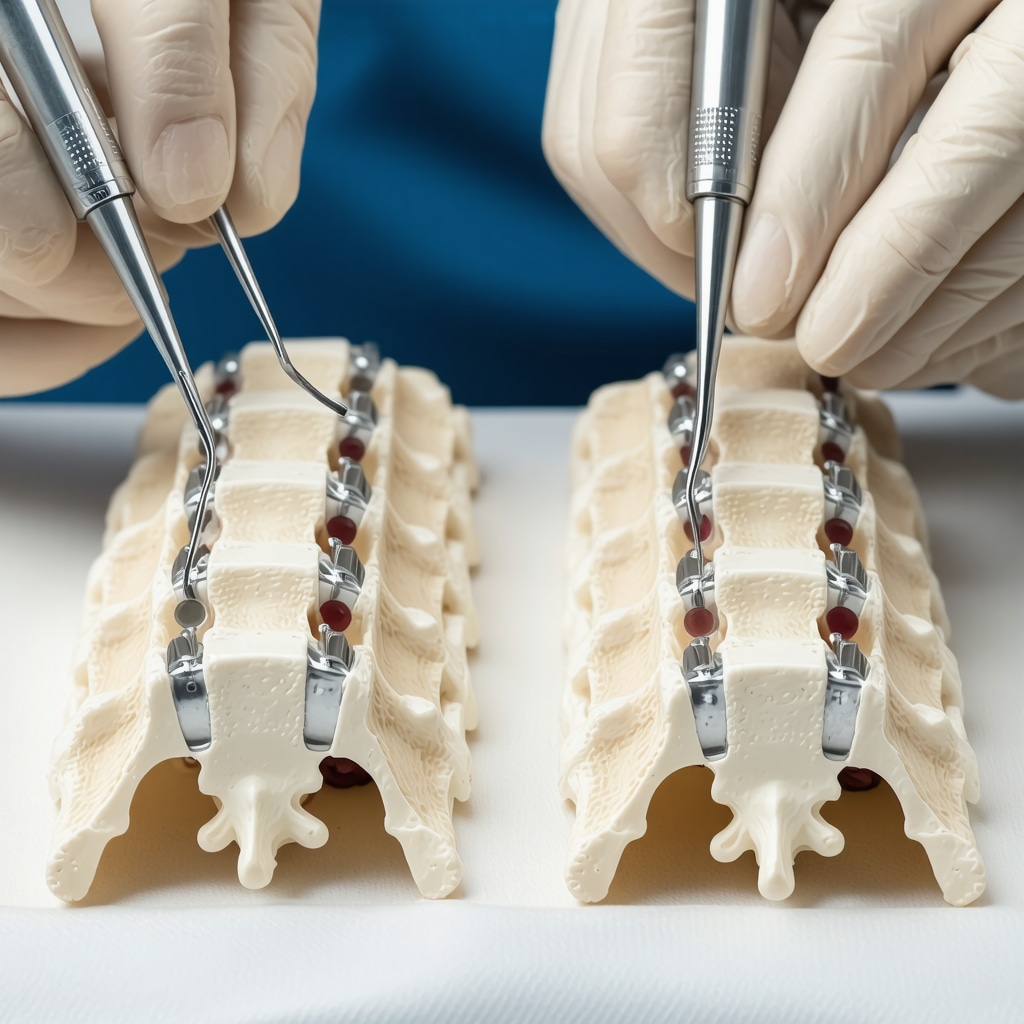
Disc resection, often performed via microdiscectomy or minimally invasive techniques, aims to excise herniated nucleus pulposus material while preserving spinal segment mobility. This procedure mitigates nerve root compression with reduced operative trauma. However, it is essential to acknowledge that disc resection does not address underlying segmental instability or advanced degenerative changes, which may predispose patients to recurrent symptoms or progressive spondylosis.
Fusion Surgery: Restoring Stability at the Expense of Mobility
Spinal fusion involves arthrodesis of vertebral segments to eliminate pathological motion, thereby providing robust mechanical stabilization. This approach is particularly indicated in cases of segmental instability, deformity, or multi-level degenerative disease. While fusion can yield durable pain relief, it inherently sacrifices physiological segmental mobility, potentially accelerating adjacent segment degeneration. New Jersey specialists highlight that patient selection and surgical technique refinement are paramount to optimizing outcomes and mitigating these risks, as detailed in comprehensive fusion surgery insights.
What are the nuanced criteria NJ spine surgeons use to decide between disc resection and fusion surgery?
Decision-making hinges on a multifactorial assessment including diagnostic imaging revealing disc pathology extent, segmental instability evidenced by dynamic radiographs, neurological deficits, and patient comorbidities. In nuanced scenarios, minimally invasive microdiscectomy may be favored for contained herniations with preserved segmental stability, while fusion is reserved for patients exhibiting spondylolisthesis, recurrent disc herniations, or significant degenerative facet arthropathy. Expert panels in NJ also consider patient activity demands and risk tolerance to customize surgical plans effectively.
Integrating Technological Advances and Patient-Centered Outcomes in NJ Spine Surgery
Emerging techniques such as robotic-assisted spine surgery and advanced imaging modalities are increasingly incorporated to enhance precision in both disc resection and fusion procedures. These innovations contribute to reducing intraoperative risks and improving recovery trajectories. NJ spine surgeons advocate for a holistic treatment paradigm that balances surgical intervention with adjunctive rehabilitation, as outlined in resources on postoperative recovery gear recommendations.
For patients and practitioners seeking comprehensive, evidence-based guidance on spinal surgery options, engaging with board-certified experts is imperative. Explore how to identify qualified specialists through our detailed guide on finding board-certified spine surgeons in NJ.
Authoritative Reference: According to a review in the Journal of Neurosurgery: Spine, surgical decision-making for lumbar disc herniation must balance decompression needs with preservation of spinal biomechanics to optimize patient outcomes over the long term.
Engage with NJ Spine Surgery Experts: If you are a healthcare professional or patient interested in deeper clinical insights or sharing your experiences with disc resection versus fusion surgery, consider contributing to our expert discussions and accessing advanced resources on spinal care.
Evaluating Long-Term Functional Outcomes and Quality of Life
Beyond immediate surgical success, assessing the long-term functional outcomes and quality of life after disc resection or fusion surgery is crucial. New Jersey spine surgeons emphasize patient-reported outcome measures (PROMs) as an essential tool for capturing nuanced recovery trajectories. Patients undergoing disc resection often experience faster return to activity due to preserved segmental motion, but may face recurrent symptoms if underlying instability is unaddressed. Conversely, fusion surgery provides lasting stability, yet the loss of mobility can impact overall spinal biomechanics, sometimes leading to compensatory discomfort in adjacent segments.
Integrating PROMs with objective clinical data enables surgeons to tailor postoperative rehabilitation and anticipate potential complications early, improving holistic care. Exploring these outcomes helps refine patient counseling and align surgical choices with individualized expectations.
Emerging Role of Motion-Preserving Techniques: Beyond Traditional Fusion
In response to concerns about mobility loss following fusion, motion-preserving technologies such as artificial disc replacement (ADR) have gained attention in specialized NJ centers. ADR aims to maintain spinal kinematics while alleviating nerve compression, offering an alternative for select patients with single-level disc disease without instability. Although long-term data is still evolving, early studies suggest that ADR may reduce adjacent segment degeneration compared to fusion.
However, candidacy for ADR is stringent, and expert evaluation is necessary to balance benefits against risks such as implant wear or subsidence. Patients interested in exploring these options should consult with board-certified specialists experienced in advanced spine technologies, which can be found through dedicated NJ surgeon directories.
How Do New Jersey Spine Surgeons Integrate Patient Lifestyle Factors into Surgical Planning?
Expert practitioners recognize that surgical outcomes extend beyond anatomical correction to encompass patient-specific lifestyle demands, occupational needs, and activity levels. For example, athletes or physically active individuals may prioritize motion preservation, favoring disc resection or ADR, whereas patients with manual labor occupations and significant instability might benefit more from fusion to ensure durable spinal integrity.
Additionally, psychosocial factors such as pain tolerance, mental health status, and support systems are increasingly incorporated into shared decision-making models. This comprehensive approach enhances patient satisfaction and adherence to postoperative protocols, ultimately influencing success rates.
Synthesizing Evidence and Expert Consensus for Informed Choices
Recent systematic reviews and meta-analyses published in the Spine Journal reinforce the importance of individualized treatment algorithms that consider disc pathology severity, segmental stability, and patient-centered factors. This evidence base supports the nuanced frameworks employed by NJ spine surgeons, blending cutting-edge research with clinical expertise.
For patients navigating complex spine surgery decisions, exploring resources such as signs indicating surgical intervention can provide clarity on timing and appropriateness, facilitating proactive engagement with healthcare providers.
Join the Conversation: Share your experiences or questions about disc resection versus fusion surgery in the comments below. Your insights can enrich this expert community and help others facing similar choices.
Nuanced Integration of Biomechanical Modeling and Personalized Surgical Planning
Cutting-edge biomechanical modeling tools are increasingly employed by New Jersey spine surgeons to simulate postoperative spinal kinematics and stress distributions following either disc resection or fusion. These sophisticated computational analyses enable a predictive understanding of how altered segmental mechanics may impact adjacent levels and overall spinal balance. By integrating patient-specific imaging data such as high-resolution MRI and dynamic fluoroscopy into finite element models, surgeons can forecast potential complications like accelerated adjacent segment degeneration or implant failure.
This predictive capability sharpens surgical planning, allowing for customized approaches that optimize structural preservation without compromising neural decompression. The integration of such technologies represents a leap beyond traditional decision-making paradigms, anchoring interventions in both clinical expertise and biomechanical science.
How do biomechanical simulations influence the choice between disc resection and fusion in complex degenerative cases?
In complex cases featuring multi-level degeneration or borderline instability, biomechanical simulations help delineate whether motion preservation is viable or if fusion is essential for stability. For instance, simulations may reveal that disc resection alone could jeopardize segmental integrity in the presence of facet joint arthropathy, prompting a fusion recommendation. Conversely, when simulations predict minimal biomechanical disruption, surgeons may confidently pursue less invasive, motion-sparing procedures.
Such insights not only refine surgical indications but also contribute to shared decision-making, as patients are presented with individualized risk-benefit profiles grounded in quantitative data.
Advanced Neurophysiological Monitoring: Enhancing Safety and Precision During Surgery
Intraoperative neurophysiological monitoring (IONM) has become a cornerstone in NJ spine surgeries, particularly when weighing the risks of nerve root manipulation during disc resection or the biomechanical alterations after fusion. Techniques such as somatosensory evoked potentials (SSEPs) and motor evoked potentials (MEPs) provide real-time feedback on neural pathway integrity, enabling immediate adjustments to surgical maneuvers.
This vigilant monitoring mitigates the risk of iatrogenic neurological injury, especially in anatomically challenging cases or when performing multi-level fusion. The deployment of IONM exemplifies an expert-level commitment to patient safety and functional preservation, aligning with best-practice protocols endorsed by the American Association of Neurological Surgeons.
Leveraging Postoperative Analytics and Machine Learning for Outcome Optimization
Beyond intraoperative advances, New Jersey spine centers are pioneering the use of machine learning algorithms to analyze large datasets of postoperative outcomes. By correlating variables such as surgical technique, patient demographics, comorbidities, and PROMs, these models aim to predict individualized recovery trajectories and complication risks.
For example, machine learning classifiers can identify patients at higher risk for pseudoarthrosis after fusion or recurrent herniation following disc resection. These predictive insights empower clinicians to tailor follow-up regimens, intensify rehabilitation protocols, or reconsider surgical candidacy preemptively.
As this data-driven approach matures, it promises to transform spine surgery from a predominantly experience-based practice to one underpinned by precision medicine.
Authoritative Reference: A landmark study published in Spine Journal (2019) demonstrates the efficacy of finite element modeling in predicting postoperative biomechanical outcomes, endorsing its integration into pre-surgical planning workflows.
Engage with NJ Spine Surgery Experts: Are you interested in how biomechanical modeling or neurophysiological monitoring can optimize your surgical plan? Connect with our board-certified specialists for an in-depth consultation tailored to your unique spinal health profile.
Harnessing Predictive Biomechanics for Tailored Surgical Interventions
The integration of patient-specific finite element analysis in preoperative planning is revolutionizing how New Jersey spine surgeons approach complex spinal pathologies. By simulating postoperative biomechanical environments, these models forecast stress redistribution not only at the index level but also at adjacent segments, allowing for nuanced decisions between preserving motion via disc resection or ensuring stability through fusion.
Such advanced simulations incorporate variables like facet joint degeneration, ligamentous integrity, and vertebral alignment, transcending traditional imaging assessments. This level of precision aids in minimizing postoperative complications such as adjacent segment disease or implant subsidence, optimizing long-term spinal health.
How do biomechanical simulations influence the choice between disc resection and fusion in complex degenerative cases?
In multifactorial spinal degeneration scenarios, biomechanical modeling delineates the thresholds at which segmental mobility compromises stability. For example, when simulations exhibit elevated shear forces or abnormal segmental motion post-resection, fusion becomes the preferred modality. Conversely, stable biomechanical profiles support less invasive, motion-preserving options. This data-driven stratification supports evidence-based, patient-centered surgical planning.
Neurophysiological Monitoring: An Essential Layer of Intraoperative Safety and Precision
Intraoperative neurophysiological monitoring (IONM), including somatosensory evoked potentials and motor evoked potentials, provides a real-time functional map of neural structures during surgical manipulation. Especially in anatomically complex or revision surgeries, IONM enables immediate detection of neural compromise, permitting intraoperative modifications that preserve neurological function.
This modality is indispensable during both disc resection and fusion procedures, mitigating risks of iatrogenic injury, particularly in high-risk patients or multi-level interventions. Its adoption aligns with the stringent safety standards advocated by the American Association of Neurological Surgeons and reflects a sophisticated commitment to optimizing patient outcomes.
Machine Learning and Postoperative Analytics: The Frontier of Personalized Spine Surgery
Emerging machine learning frameworks analyze extensive postoperative datasets, correlating patient demographics, surgical parameters, and longitudinal recovery metrics. These algorithms identify predictors of complications such as pseudoarthrosis, recurrent herniation, or chronic pain syndromes, enabling proactive clinical interventions.
By stratifying patients according to individualized risk profiles, clinicians can customize rehabilitation intensity, monitoring frequency, and even reconsider surgical candidacy. This approach epitomizes the shift towards precision medicine in spine surgery, promising enhanced functional recovery and patient satisfaction.
Authoritative Reference: A seminal publication in the Spine Journal (2019) validates the predictive accuracy of finite element modeling in pre-surgical biomechanical assessment, underscoring its clinical utility.
Engage with NJ Spine Surgery Experts: Are you intrigued by how biomechanical modeling, neurophysiological monitoring, or data-driven analytics can refine your surgical strategy? Connect directly with our board-certified specialists for advanced consultations tailored to your spinal health needs.

Expert Insights & Advanced Considerations
Biomechanical Modeling as a Cornerstone for Personalized Spine Surgery
Leveraging patient-specific finite element analyses allows NJ spine surgeons to simulate postoperative stress and motion dynamics, providing a predictive framework that guides the choice between disc resection and fusion. This approach transcends conventional imaging by quantifying segmental stability thresholds, helping to mitigate risks such as adjacent segment degeneration or implant failure.
The Critical Role of Intraoperative Neurophysiological Monitoring (IONM)
Real-time neural integrity assessment via somatosensory and motor evoked potentials elevates surgical precision and safety in complex cases. IONM facilitates immediate intraoperative adjustments, reducing iatrogenic nerve injury risk during both disc resection and fusion procedures, especially in multi-level or revision surgeries.
Machine Learning-Driven Outcome Prediction Enhances Postoperative Care
Integrating machine learning analytics with large postoperative datasets enables identification of patient-specific risk factors for complications like pseudoarthrosis or recurrent herniation. This empowers NJ specialists to customize follow-up protocols and rehabilitation strategies, advancing spine surgery into the realm of precision medicine.
Incorporating Lifestyle and Psychosocial Variables in Surgical Planning
Beyond anatomical factors, expert surgeons in New Jersey emphasize tailoring surgical decisions by factoring in patient activity levels, occupational demands, and psychosocial status. This holistic model improves patient satisfaction and adherence, ultimately influencing long-term outcomes after disc resection or fusion surgery.
Curated Expert Resources
Journal of Neurosurgery: Spine – Offers comprehensive peer-reviewed studies on spinal biomechanics and surgical outcomes, vital for cutting-edge surgical decision-making.
Spine Journal – Publishes systematic reviews and meta-analyses elucidating evidence-based algorithms for managing lumbar disc pathologies.
American Association of Neurological Surgeons (AANS) Guidelines – Provides authoritative protocols on intraoperative neurophysiological monitoring standards to ensure patient safety.
NJ Spine Surgeons Online Portal – An indispensable resource linking to detailed insights on fusion surgery, minimally invasive techniques, and postoperative care essentials (fusion surgery insights, recovery gear recommendations).
Recent Biomechanical Modeling Studies (Spine Journal, 2019) – Validates finite element modeling’s predictive capacity in pre-surgical planning, essential reading for integrating advanced analytics into practice.
Final Expert Perspective
The evolving paradigm of disc resection versus fusion surgery in New Jersey underscores a sophisticated interplay of biomechanical science, real-time neural monitoring, and data-driven postoperative management. Expert spine surgeons champion an individualized, evidence-based strategy that balances motion preservation with mechanical stability, tailored to each patient’s unique anatomical and lifestyle context. Embracing technological innovations such as finite element modeling and machine learning analytics refines surgical precision and optimizes long-term functional outcomes. For those navigating these complex decisions, engaging with board-certified specialists and exploring comprehensive resources can profoundly enhance both understanding and care quality. To deepen your insight or to consult with New Jersey’s leading spine experts, consider visiting our contact page or explore how to identify top-tier practitioners through our guide to finding board-certified spine surgeons.

This post offers fantastic insights into the nuanced decision-making process for choosing between disc resection and fusion surgery. From my experience working with NJ spine surgeons, I’ve seen how critical patient-specific factors are in guiding these choices—especially when considering biomechanical analysis and lifestyle demands. I find the integration of advanced imaging and biomechanical simulations particularly fascinating, as they seem to provide a more predictive approach to outcomes. One challenge I’ve noticed is balancing the desire for motion preservation with the risk of recurrent instability, especially in patients with borderline degeneration. I wonder, for those who have gone through either procedure, how did your long-term recovery and functionality compare? Are there specific factors or signs that helped determine which path was ultimately better suited for your condition? Overall, I believe continued advancements like machine learning and intraoperative monitoring will further refine these individualized approaches, ultimately improving patient satisfaction and results.
This article offers a comprehensive look at the delicate balance surgeons consider when choosing between disc resection and fusion. Having experienced back issues myself, I particularly appreciate how the article highlights the importance of individualized assessments—something I believe can really make or break long-term satisfaction. I find the mention of biomechanical modeling especially intriguing; it seems like a powerful way to predict outcomes and personalize treatment plans. That said, I’m curious about the potential downsides or limitations of relying heavily on these advanced technologies. For example, how do surgeons ensure that models accurately reflect complex biological realities? Also, with the rising use of motion-preserving procedures like artificial disc replacement, is there enough long-term data to support their widespread application? I’m interested in hearing from others—have you or someone you know undergone these procedures? How did the recovery and functional outcomes compare, especially over multiple years? Overall, I believe these technological advances are promising, but continued research and patient-centered planning remain key.