Exploring Chronic Pain Solutions: Spinal Cord Stimulator or Surgery?
Living with chronic pain is a persistent challenge that affects thousands across New Jersey, often diminishing quality of life and limiting daily activities. When conservative treatments fail, patients and clinicians face a pivotal decision: opt for a spinal cord stimulator (SCS) implant or pursue more invasive surgical interventions. Understanding the nuanced differences between these options is essential for informed, personalized care.
Decoding Spinal Cord Stimulation: A Minimally Invasive Alternative
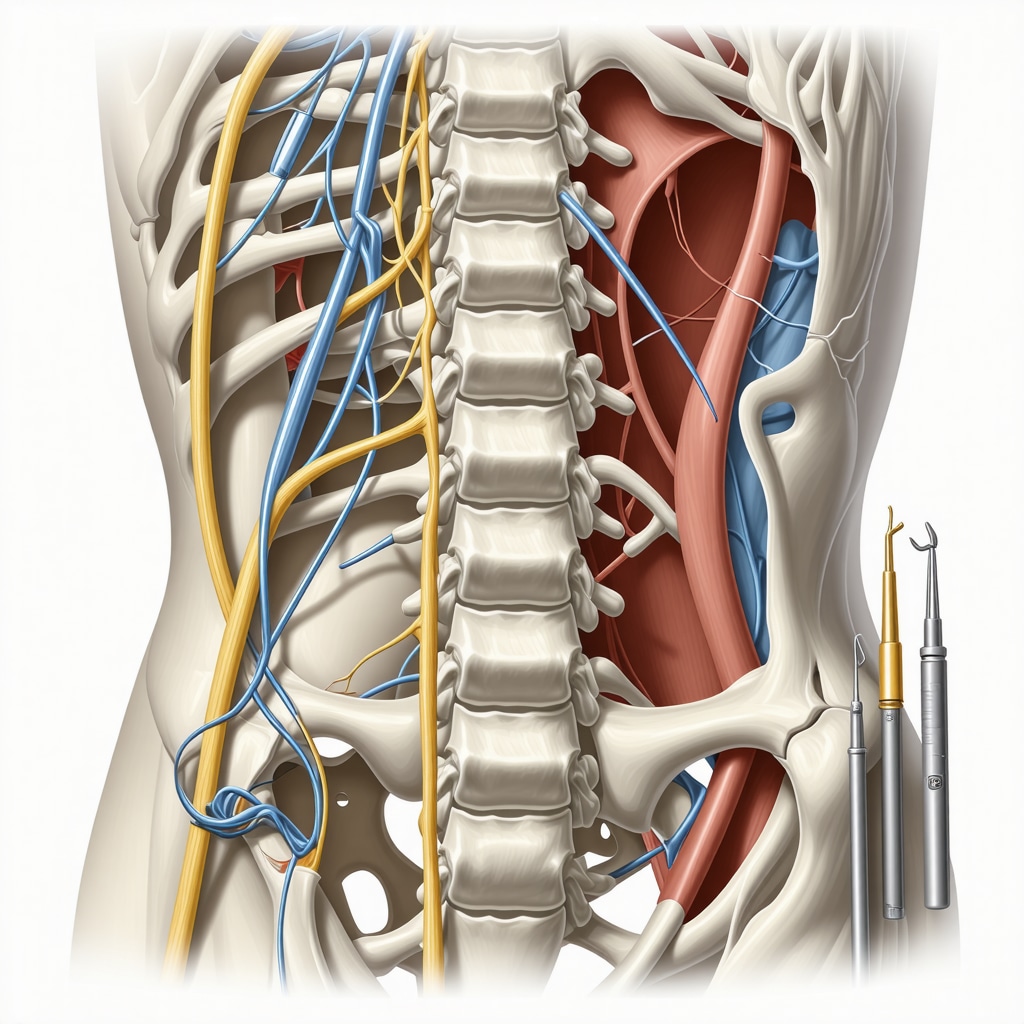
Spinal cord stimulators work by delivering electrical impulses to the spinal cord, interrupting pain signals before they reach the brain. This neuromodulation approach is particularly suited for patients whose pain stems from nerve-related causes, such as failed back surgery syndrome or complex regional pain syndrome. The procedure involves a trial period, allowing patients to experience the benefits before permanent implantation. Its minimally invasive nature offers faster recovery times and fewer risks compared to traditional surgery.
How does the effectiveness of spinal cord stimulators compare to conventional surgery in NJ patients?
Clinical studies and expert observations indicate that while SCS can significantly reduce pain and improve functionality, its success depends heavily on patient selection and underlying pathology. Surgery, such as spinal fusion or decompression, may offer a definitive solution for structural problems but carries higher risks, longer recovery, and potential complications. Patients in New Jersey often choose stimulation when surgery poses excessive risk or when pain is neuropathic rather than mechanical.
Weighing Surgical Options: When Is Surgery Unavoidable?
For certain conditions like severe spinal stenosis, herniated discs causing nerve compression, or spinal instability, surgery remains the gold standard. Advances in minimally invasive techniques have improved outcomes and reduced hospital stays, but surgery inherently involves anesthesia, tissue disruption, and a longer rehabilitation period. Surgeons in NJ emphasize thorough diagnostic evaluation — including imaging and clinical assessment — to determine candidacy for surgery versus neuromodulation.
Patient Experiences Illuminate the Decision-Making Process
Consider the case of a 58-year-old NJ resident with chronic lower back pain unrelieved by medication. After a spinal cord stimulator trial, she reported a 60% reduction in pain and resumed daily walks without discomfort. Conversely, a 45-year-old with spinal instability underwent minimally invasive fusion surgery, achieving long-term stability but requiring months of physical therapy. These contrasting experiences underscore the importance of individualized treatment plans crafted by board-certified spine specialists. To find trusted experts near you, explore how to find board-certified spine surgeons in NJ.
Integrating Expert Guidance and Cutting-Edge Research
Leading New Jersey spine centers incorporate evidence-based protocols and patient-centric approaches. According to a 2019 study published by the National Institutes of Health, spinal cord stimulation offers notable pain relief with lower complication rates compared to complex surgeries in selected patient populations. However, comprehensive evaluation including imaging, pain characterization, and functional assessment remains critical before deciding on either path.
If you’re navigating chronic pain treatment options, engaging with specialists who can elucidate the benefits and risks tailored to your condition is invaluable. For more insights on minimally invasive procedures, visit exploring minimally invasive spine surgery benefits.
What has been your experience with chronic pain treatments? Share your story or questions below to connect with others navigating similar journeys.
Listening to Your Body: The Emotional Side of Choosing Between SCS and Surgery
Living with chronic pain isn’t just a physical battle; it’s an emotional journey filled with uncertainty and hope. I remember a patient named Lisa, who faced this crossroads. She was hesitant about surgery but worried about the long-term effectiveness of spinal cord stimulators. Our conversations revealed how vital it is to address fears and expectations openly. Sometimes, the decision hinges less on medical facts and more on personal comfort with the risks and lifestyle changes involved.
Beyond the Procedure: Rehabilitation and Lifestyle Impact
One insight often overlooked is how post-treatment rehabilitation shapes outcomes. Whether you choose minimally invasive techniques or opt for a spinal cord stimulator, your commitment to physical therapy and lifestyle adjustments can make a world of difference. For example, after her SCS implantation, Lisa embraced tailored exercises that significantly improved her mobility and mood. Meanwhile, others who underwent surgery shared that the recovery period, while challenging, eventually allowed them to regain a level of freedom they thought was lost.
How do you balance medical advice and personal intuition when deciding on spine treatments?
This question often arises in my discussions with patients. Medical experts provide evidence-based recommendations, but each person’s pain journey and priorities are unique. Reflecting on this, I encourage patients to engage deeply in their treatment planning, seek multiple opinions if necessary, and listen to their instincts. As highlighted by the American Academy of Pain Medicine, collaborative decision-making enhances satisfaction and outcomes in chronic pain care.
Exploring Resources and Support in New Jersey
New Jersey offers an impressive network of spine specialists and support resources. For those considering surgery, sites like Bergen County’s leading spine surgeons provide detailed profiles and patient reviews that can guide your choice. Additionally, understanding recovery tips and managing expectations with resources such as spine surgery recovery tips for New Jersey patients can empower you throughout the healing process.
Ultimately, chronic pain treatment is deeply personal. If you’ve navigated these decisions or are currently weighing your options, I invite you to share your experiences or questions below. Your story could be the insight someone else needs today.
Precision in Patient Selection: Tailoring Spinal Cord Stimulator Use for Optimal Outcomes
While spinal cord stimulation (SCS) presents a less invasive alternative to surgery, its efficacy hinges on meticulous patient selection. Advanced diagnostic tools such as quantitative sensory testing (QST) and high-resolution functional MRI enable clinicians to better identify neuropathic pain phenotypes most likely to respond favorably to neuromodulation. Moreover, psychological assessment plays a pivotal role, as factors like catastrophizing or depression may blunt SCS effectiveness.
Innovations in programming SCS devices now allow for multiwaveform and burst stimulation patterns, providing customizable pain modulation that can address complex pain syndromes resistant to traditional tonic stimulation. This level of personalization underscores the importance of partnering with specialists experienced in neurostimulation technologies to maximize therapeutic success.
What are the emerging biomarkers that predict spinal cord stimulator success in chronic pain management?
Recent research highlights potential biomarkers such as serum inflammatory cytokines and neurophysiological markers measured by evoked potentials that correlate with positive SCS outcomes. These insights, detailed in a 2020 peer-reviewed study in The Journal of Pain, suggest a future where objective biological indicators guide personalized chronic pain interventions, reducing trial-and-error approaches.
Integrating Multimodal Therapies Post-SCS or Surgery: Enhancing Long-Term Patient Functionality
Optimal chronic pain management transcends the procedure itself. Combining SCS or surgical intervention with multidisciplinary rehabilitation—including physical therapy, cognitive behavioral therapy (CBT), and occupational therapy—can significantly improve long-term outcomes. For example, graded motor imagery and mirror therapy have shown promise in retraining the central nervous system post-intervention.
This integrative model addresses both the physiological and psychosocial dimensions of chronic pain, fostering resilience and functional restoration. Patients participating in comprehensive pain management programs report improved quality of life and reduced reliance on opioids, emphasizing the necessity of a holistic approach post-procedure.
Decoding Complex Cases: When Hybrid Approaches Combine Neuromodulation and Surgery
Some patients with multifactorial etiologies—such as combined mechanical instability and neuropathic pain—may benefit from a hybrid strategy incorporating both surgical correction and spinal cord stimulation. For instance, surgical decompression can alleviate structural nerve impingement, while subsequent SCS implantation may manage residual neuropathic symptoms.
This sequential or concurrent treatment paradigm requires nuanced clinical judgment and collaboration among spine surgeons, pain specialists, and rehabilitation therapists. Such multidisciplinary coordination is exemplified by leading centers in New Jersey, which prioritize tailored, stage-based care plans to optimize patient outcomes.
Understanding these complex clinical pathways invites patients and providers alike to consider beyond traditional binaries in chronic pain treatment.
Are you navigating chronic pain with overlapping structural and neuropathic components? Connect with our specialists to explore customized hybrid treatment options designed for your unique needs.
Innovative Neurostimulation Technologies Elevating Chronic Pain Management
Recent advancements in spinal cord stimulation (SCS) technology have revolutionized chronic pain therapy, enabling clinicians to tailor interventions with remarkable precision. Modern devices incorporate closed-loop feedback systems that dynamically adjust stimulation parameters in response to physiological signals, enhancing pain control while minimizing side effects. These intelligent stimulators represent a leap beyond traditional open-loop designs, offering personalized neuromodulation that adapts to patient activity and posture.
Collaborative Clinical Pathways: Merging Expertise for Superior Outcomes
In New Jersey, integrated care models unite spine surgeons, pain management specialists, and rehabilitation therapists to form multidisciplinary teams dedicated to complex chronic pain cases. This collaborative approach facilitates comprehensive evaluation, from advanced imaging modalities to psychosocial assessments, ensuring that treatment strategies—whether surgical, neuromodulatory, or hybrid—are optimized for each patient’s unique pathology and lifestyle needs.
How can emerging neuroimaging techniques refine candidate selection for spinal cord stimulation?
Emerging neuroimaging modalities, such as functional near-infrared spectroscopy (fNIRS) and diffusion tensor imaging (DTI), are gaining traction in the preoperative assessment of SCS candidates. These tools elucidate central nervous system alterations associated with chronic pain, enabling precise phenotyping that predicts responsiveness to neuromodulation. A 2023 study published in NeuroImage Clinical demonstrates that integrating DTI metrics with clinical variables enhances prognostic accuracy for SCS outcomes, minimizing futile trials and optimizing resource allocation.
Personalized Rehabilitation Protocols: Extending Benefits Beyond Intervention
Post-procedural rehabilitation tailored to the neuromodulatory or surgical pathway is pivotal in consolidating pain relief and functional gains. Innovative programs utilize virtual reality (VR)-assisted motor retraining and biofeedback to accelerate neuroplasticity and mitigate maladaptive pain behaviors. These sophisticated rehabilitation strategies complement the physiological effects of SCS or surgery, promoting holistic recovery and long-term quality of life improvements.
Data-Driven Decision Support Systems: Empowering Patients and Providers
Leveraging artificial intelligence and machine learning, decision support tools now assist clinicians and patients in weighing the risks and benefits of SCS versus surgery. These systems analyze extensive datasets encompassing patient demographics, imaging findings, psychosocial factors, and prior treatment responses to generate individualized prognostic profiles. Such evidence-based frameworks enhance shared decision-making, aligning therapeutic choices with patient values and clinical evidence.
Are you seeking expert guidance that integrates cutting-edge diagnostics, personalized therapies, and collaborative care for your chronic pain? Connect with New Jersey’s leading specialists to explore tailored solutions that transcend conventional treatment paradigms.

Frequently Asked Questions (FAQ)
What types of chronic pain conditions are best suited for spinal cord stimulation?
Spinal cord stimulation (SCS) is most effective for neuropathic pain syndromes such as failed back surgery syndrome, complex regional pain syndrome, and certain radiculopathies. It is less suited for purely mechanical or structural pain without a neuropathic component. Proper diagnostic evaluation is essential to identify candidates who will benefit the most.
How do spinal cord stimulators compare to surgery in terms of risks and recovery?
SCS implantation is minimally invasive, generally associated with lower procedural risks, shorter hospital stays, and faster recovery compared to traditional spine surgery. Surgery, while potentially offering a definitive correction of structural pathology, involves higher risks related to anesthesia, tissue disruption, and longer rehabilitation periods.
Can spinal cord stimulation be combined with surgery for complex cases?
Yes, hybrid approaches are sometimes employed when patients have both mechanical instability and neuropathic pain. Surgery may address the structural issue, followed by SCS implantation to manage residual neuropathic symptoms. Such combined strategies require multidisciplinary coordination for optimal outcomes.
What role do psychological factors play in the success of spinal cord stimulation?
Psychological factors such as depression, anxiety, and pain catastrophizing can influence SCS outcomes. Comprehensive preoperative psychological assessment and support improve the likelihood of successful neuromodulation by addressing these modifiable factors.
How have recent technological advancements improved spinal cord stimulation?
Modern SCS devices feature closed-loop feedback, multiwaveform programming, and burst stimulation, allowing personalized modulation tailored to patient activity and pain patterns. These innovations enhance pain relief efficacy and reduce side effects compared to earlier open-loop systems.
What rehabilitation strategies enhance recovery after SCS or spine surgery?
Multimodal rehabilitation combining physical therapy, cognitive behavioral therapy, and occupational therapy supports functional restoration and pain management. Emerging techniques such as virtual reality-assisted motor retraining and biofeedback promote neuroplasticity and improve long-term outcomes.
Are there biomarkers or imaging techniques that predict who will benefit from SCS?
Emerging research identifies inflammatory cytokines, neurophysiological evoked potentials, and advanced neuroimaging modalities like diffusion tensor imaging as promising predictors of SCS responsiveness. These tools help refine patient selection, reducing ineffective trials.
How can patients in New Jersey find trusted specialists for chronic pain treatment?
New Jersey offers a network of board-certified spine surgeons and pain specialists who utilize evidence-based, multidisciplinary approaches. Resources such as local spine surgeon directories and patient reviews can guide patients in selecting experienced providers tailored to their needs.
What factors should patients consider when choosing between SCS and surgery?
Patients should weigh the nature of their pain (neuropathic vs mechanical), overall health, psychological readiness, potential risks, recovery expectations, and lifestyle goals. Shared decision-making with multidisciplinary teams ensures treatment aligns with individual values and clinical evidence.
Is spinal cord stimulation a permanent solution for chronic pain?
While SCS can provide long-term pain relief, it is not necessarily curative. Device programming adjustments and ongoing rehabilitation are often needed, and some patients may eventually require additional interventions. Continuous follow-up is essential for sustained benefit.
Trusted External Sources
- National Institutes of Health (NIH) – PubMed Central: Offers peer-reviewed clinical studies on spinal cord stimulation efficacy and safety, providing evidence-based insights critical for clinical decision-making.
- American Academy of Pain Medicine (AAPM): Provides guidelines on multidisciplinary pain management, psychological assessment, and evidence-based neuromodulation therapies.
- Journal of Pain: A leading peer-reviewed journal publishing cutting-edge research on biomarkers, neurophysiology, and innovative chronic pain therapies including spinal cord stimulation.
- NeuroImage Clinical: Publishes advanced neuroimaging studies that refine candidate selection and prognostication for neuromodulation interventions.
- New Jersey Spine Society and Local Medical Boards: Offer reliable directories and patient resources to locate board-certified spine surgeons and pain specialists within NJ, facilitating access to expert care.
Conclusion
Deciding between spinal cord stimulation and surgery for chronic pain in New Jersey requires an expert, individualized approach that integrates detailed diagnostics, patient-specific factors, and evolving technological advances. Spinal cord stimulators provide a minimally invasive, customizable option particularly suited for neuropathic pain, while surgery remains indispensable for correcting structural spinal pathologies. Collaborative multidisciplinary care, incorporating cutting-edge neuroimaging, psychological evaluation, and tailored rehabilitation, optimizes outcomes and quality of life. Patients are encouraged to engage deeply with board-certified specialists, explore all treatment avenues, and participate actively in shared decision-making. By leveraging this knowledge, individuals living with chronic pain can pursue informed choices that align with their unique clinical needs and personal goals.
Explore related expert content, share your experiences, or reach out to specialists to empower your chronic pain journey today.


The post does a great job highlighting how spinal cord stimulators (SCS) provide a less invasive option compared to surgery for certain kinds of chronic neuropathic pain. What really strikes me is the emphasis on personalized treatment plans and the importance of comprehensive diagnostics, including psychological evaluations. From what I’ve seen in friends and family navigating chronic pain, the psychological aspect is often overlooked but can profoundly affect outcomes, especially with SCS effectiveness. The hybrid approach combining surgery and neuromodulation also seems promising for those with overlapping mechanical and neuropathic issues, which is an intriguing development I hadn’t thought much about before. It makes me wonder, how extensive is the availability of such multidisciplinary teams in New Jersey? Are most patients able to access these collaborative care models, or is this limited to a few specialized centers? Also, for someone weighing these options, balancing the uncertainty of outcomes against recovery time and lifestyle impact must be daunting. I’m curious how others have approached the emotional side of deciding between neuromodulation and surgery, especially when the science offers guidance but no absolute answers.
Melissa, you raise an excellent point about the availability and accessibility of multidisciplinary teams in New Jersey for chronic pain management. From what I’ve gathered volunteering with local health organizations, while New Jersey has several specialized centers that offer integrated care models combining spine surgeons, pain specialists, and rehab therapists, these tend to be concentrated in metropolitan areas like Bergen County or Newark. Patients in more rural or underserved regions might face barriers accessing such comprehensive teams, resulting in less coordinated care. Beyond geographic factors, insurance coverage also influences the extent to which patients can tap into multidisciplinary resources. Regarding the emotional challenge you mentioned when deciding between spinal cord stimulation and surgery, I think it’s crucial patients receive mental health support alongside medical consultations. Chronic pain often affects mood and decision-making capacity, so psychological counseling can help patients reconcile the risks and benefits on a personal level. Has anyone else found that including a mental health professional as part of their care team helped ease the anxiety of making such treatment choices? It seems we might benefit from wider adoption of collaborative care that explicitly addresses both the physical and emotional complexities inherent in chronic pain interventions.
Jonathan, I appreciate your insight into how multidisciplinary teams in New Jersey are often concentrated in larger metropolitan areas, which can create access challenges for patients elsewhere. In my experience assisting a relative dealing with complex regional pain syndrome (CRPS), coordinating care between specialists was a major hurdle. Although we eventually connected with a team offering both neuromodulation options and surgical consultation, it took time and persistence. I also agree that integrating mental health support is vital—chronic pain can be mentally exhausting and anxiety around treatment choices often exacerbates the situation.
One thing not to overlook is the role of telemedicine, which some New Jersey centers have started using to bridge geographic gaps. Virtual consultations with pain psychologists or rehabilitation therapists have helped provide continuous support, even when in-person visits weren’t feasible. I wonder if expanding these remote services might improve equitable access to comprehensive care, especially for those balancing insurance constraints and travel limitations.
For anyone navigating this difficult decision, how are you balancing the availability of multidisciplinary care with the emotional toll and logistical challenges? Have you found telehealth or community resources a useful complement during your journey? It would be great to hear how different patients and caregivers make these complex choices manageable while aiming for the best outcomes.
Building on the insightful discussion about multidisciplinary teams in New Jersey, I’ve observed firsthand how pivotal such collaborative care can be for chronic pain patients. Unfortunately, the availability does seem heavily skewed towards larger urban centers, which doesn’t always help those living outside metropolitan hubs. The role of telemedicine, as previously mentioned, is an encouraging development to bridge this gap, especially for mental health support and physical therapy follow-ups.
From a personal perspective, I’ve known someone who underwent a spinal cord stimulator implantation after years of neuropathic pain. What stood out was how crucial the psychological assessment and support were for her journey—not only in alleviating anxiety about the procedure but also in enhancing the overall effectiveness of the treatment. Insights from the post about how factors like depression or pain catastrophizing can diminish SCS outcomes resonated deeply.
It strikes me that integrating AI-driven decision support systems could greatly assist patients to navigate these complex treatment decisions, offering personalized prognostic information alongside human expertise. However, patient comfort with technology and sufficient provider education to interpret these tools remain challenges.
How are others finding ways to combine technological advancements with compassionate, accessible care—especially outside large cities? And, for folks who have faced this crossroads, how did balancing clinical advice with personal intuition influence your final choice between neuromodulation and surgery?
Reading through the post and the insightful discussion here, I’m struck by how critical patient selection truly is in determining whether a spinal cord stimulator or surgery offers the best chance for pain relief. The minimally invasive nature of SCS is appealing, especially given the faster recovery and fewer risks, but as noted, it clearly isn’t a one-size-fits-all solution. I appreciate the mention of psychological factors like depression and anxiety potentially affecting SCS effectiveness — it highlights how chronic pain care really must be holistic. I wonder if more patients could benefit from pre-treatment counseling to better set expectations and manage the emotional rollercoaster of chronic pain decision-making.
In my experience supporting a family member going through spinal fusion surgery in NJ, the recovery period was arduous but ultimately rewarding as it addressed a mechanical instability causing severe pain. However, I did notice how much they wished there was a clearer way to assess whether SCS could have been tried first. Perhaps the emerging biomarkers and advanced imaging techniques discussed in this post will help reduce trial-and-error approaches and lead to more personalized interventions.
I’m curious to know how widespread the access to these advanced diagnostic tools is across different NJ healthcare facilities. For patients outside major metro areas, does the lack of such resources delay or complicate their treatment options? Also, how do patients reconcile their personal intuition with clinical advice, especially when facing the uncertainty inherent in these complex choices?
Reading through the detailed comparison of spinal cord stimulators (SCS) and surgery for chronic pain in New Jersey really highlights how important personalized care is in this field. I was particularly interested in the discussion about the role of psychological assessment in predicting SCS success. From what I’ve observed with a friend who underwent SCS implantation, the mental health support before and after the procedure made a significant difference—not just in pain management, but also in coping with the emotional challenges of chronic pain. It’s impressive how advanced diagnostic tools like quantitative sensory testing and functional MRI are helping tailor treatment, but I wonder about their accessibility. For patients outside major NJ metro areas, is there equitable access to these cutting-edge evaluations? Additionally, since the post mentions the hybrid approach using surgery combined with SCS for complex cases, I’m curious about how the coordination among specialists is managed practically. How do patients navigate multidisciplinary teams if they live far from urban centers? It seems telemedicine might be part of the solution, but how widespread is its use in post-treatment rehabilitation specifically for spine care in NJ? I’d love to hear about others’ experiences balancing these advanced but complex options, especially when factoring in not only physical recovery but also emotional well-being.
Following the detailed discussion here, one aspect that I find particularly nuanced is the role of rehabilitation post-intervention, whether after spinal cord stimulator implantation or surgery. The post rightly emphasizes how patient commitment to tailored physical therapy and lifestyle changes can make a substantial difference in long-term outcomes. From what I’ve observed through family members’ experiences, it’s not just about the procedure itself but how well patients engage with multidisciplinary rehab programs—including physical therapy and even cognitive behavioral strategies—to rebuild function and manage pain holistically.
I was especially intrigued by the mention of virtual reality-assisted motor retraining and biofeedback techniques in rehabilitation. These emerging tools seem promising for enhancing neuroplasticity and mitigating maladaptive pain responses, but I wonder how widely available such advanced rehabilitation approaches are across New Jersey, particularly outside major medical centers.
Given the complex interplay between physiological and psychosocial factors in chronic pain management, does anyone have insight into how rehabilitation teams coordinate integrating these novel therapies with standard care? Also, for those who’ve undergone these treatments, how significant was the role of lifestyle adjustments—like exercise or sleep hygiene—in complementing medical interventions and optimizing pain relief? Sharing experiences could shed light on practical strategies that go beyond the procedural decision itself.