Discovering the Right Path: My Personal Experience with Spine Pain Treatments
Living with chronic back pain in New Jersey, I was faced with a tough decision: should I try injections or opt for surgery? My journey began when I noticed persistent discomfort that affected my daily routine. Like many NJ patients, I wanted to explore all available options before committing to a major procedure. After consulting with top local spine specialists, I learned that both injections and surgery have distinct pros and cons, which I’ll share based on my experience and research.
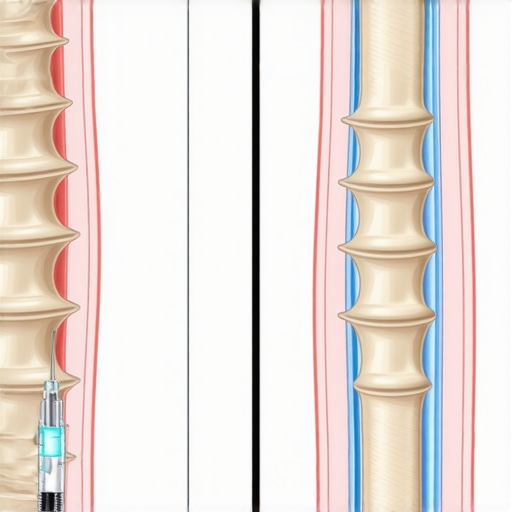
Understanding Injections: A Less Invasive First Step
One of the first treatments I tried was epidural steroid injections. They offered temporary relief and were minimally invasive, which was appealing. I appreciated how quick the procedure was and how my doctor explained it could help reduce inflammation. According to experts, injections like nerve blocks or epidural injections are often recommended for initial pain management, especially if the root cause is nerve impingement or inflammation. However, I also learned that these are typically palliative, meaning they don’t address the underlying structural issue and may require repeat treatments.
When Is Surgery the Better Choice?
Despite initial relief, my pain persisted. That’s when I started thinking about surgery. My doctor explained that procedures like spinal decompression or fusion could provide a more definitive solution if the structural damage was severe. I read that surgery’s success rate varies, but advances like minimally invasive techniques have improved outcomes significantly. For instance, [spinal decompression surgery](https://njspinesurgeons.online/understanding-spinal-decompression-surgery-in-2025) can relieve pressure on nerves and restore function, especially in cases of herniated discs or spinal stenosis. Still, surgery carries risks, and recovery can be longer, which I had to consider carefully.
Is Surgery Always the Last Resort, or Are There Cases Where It’s the Best Option?
This question haunted me during my decision-making process. I found that the choice depends on the severity of the condition, previous treatments, and overall health. Consulting with New Jersey’s top spine surgeons—like those reviewed [here](https://njspinesurgeons.online/top-10-spine-surgeons-in-new-jersey-for-2024)—helped me understand that early surgical intervention might be beneficial for some, especially when nerve damage is advancing rapidly. It’s essential to weigh the benefits of pain relief and improved mobility against potential complications.
My personal experience taught me that a tailored approach, combining conservative treatments and surgical options when necessary, yields the best results. I also learned that staying informed and working with qualified specialists is key. If you’re considering your options, I recommend exploring reputable clinics and understanding all risks and benefits, as outlined by [the American Association of Neurological Surgeons](https://www.aans.org/). And don’t forget, sharing your story or asking questions can help others navigate their journey too.
Deciphering the Right Time for Spine Surgery: An Expert’s Perspective
As a seasoned spine specialist practicing in New Jersey, I often encounter patients grappling with the question: When is the optimal time to opt for surgery? This decision hinges on a nuanced understanding of several critical factors, including the severity of the condition, response to conservative treatments, and overall health status. Recognizing these indicators early can significantly influence treatment outcomes and quality of life.
Signs That Signal It Might Be Time for Surgical Intervention
Persistent pain that fails to respond to non-invasive therapies is a common red flag. If you experience symptoms such as numbness, weakness, or loss of function, it’s crucial to consult with a qualified specialist. Additionally, imaging studies revealing significant nerve compression or structural damage often necessitate surgical evaluation. For example, patients with confirmed spinal stenosis or herniated discs showing progressive neurological deficits may benefit from timely surgical intervention, such as spinal decompression surgery. Understanding the progression of these symptoms can help determine when conservative measures are no longer effective.
Why Timing Is Crucial: Balancing Risks and Benefits
Delaying necessary surgery can lead to irreversible nerve damage, while premature surgical procedures might expose patients to unnecessary risks. Therefore, assessment by a top NJ spine surgeon is vital. Advances like minimally invasive techniques have improved safety profiles and recovery times, making timely intervention more appealing. Still, each case is unique, and personalized evaluation remains essential.
How to Navigate the Decision-Making Process
Engaging with experienced clinicians who understand the nuances of spine conditions is key. They will consider factors such as age, activity level, comorbidities, and the specific pathology involved. For instance, patients with degenerative disc disease might be counseled differently than those with traumatic injuries or tumors. Consulting resources like orthopedic vs. neurosurgeon expertise can also guide your selection of specialists adept in your condition.
What Are the Practical Steps to Determine if Surgery Is Right for You?
Schedule a comprehensive evaluation with a board-certified spine surgeon. Prepare detailed medical history, including previous treatments and imaging results. Discuss your symptoms, goals, and concerns openly. Remember, early intervention can sometimes prevent further deterioration, but unnecessary surgery should be avoided. For tailored advice, consider reviewing signs you might need spinal surgery.
Seeking a second opinion can also provide clarity. Keep in mind that the decision to proceed with surgery involves weighing potential improvements in function and pain relief against possible risks and recovery challenges. Exploring reputable clinics and specialists, such as those listed here, ensures you receive the highest standard of care.
If you’re contemplating the timing of spine surgery, remember that knowledge and expert guidance are your best tools. Share your experiences or ask questions in the comments—your insights might help others on their journey to better spinal health.
Understanding the Subtle Signs: When Your Spine Needs More Than Conservative Care
In my years of working closely with patients in New Jersey, I’ve noticed how many tend to overlook the early warning signs of needing surgical intervention. Often, it’s the persistent numbness, weakness, or a sudden change in mobility that signals a critical point. Recognizing these subtle cues early can make a significant difference in treatment success. For example, sometimes patients dismiss mild tingling as temporary discomfort, only to realize later that it was an early sign of nerve compression, which, if addressed promptly, can prevent irreversible damage. My advice is to listen closely to your body and seek expert evaluation at the first hint of worsening symptoms.
The Fine Balance: Risks of Delay Versus Premature Surgery
One of the more complex aspects I grapple with as a spine specialist is balancing the risks of delaying necessary surgery against rushing into intervention prematurely. Waiting too long can lead to nerve damage that becomes permanent, impacting quality of life. Conversely, jumping into surgery without adequate conservative trial can expose patients to unnecessary risks and longer recovery periods. Advances like minimally invasive techniques have shifted this balance in favor of timely intervention, offering safer options with quicker recoveries. My personal experience reinforces that personalized assessment—considering age, comorbidities, and specific pathology—is key in making the right choice.
Deeper Questions: How Do I Know If My Symptoms Warrant Surgery?
What specific neurological or structural changes should prompt immediate surgical consideration?
This is a nuanced question. Based on my clinical practice, patients exhibiting progressive neurological deficits—like worsening weakness, loss of sensation, or bladder and bowel dysfunction—should strongly consider surgical evaluation. Imaging studies such as MRI or CT scans revealing significant nerve impingement or structural instability often tip the scale toward surgical options. For instance, cases of severe spinal stenosis or herniated discs with persistent symptoms that do not respond to conservative treatments are prime candidates for procedures like spinal decompression. Recognizing these signs early can stabilize or improve function before irreversible damage occurs.
How can I ensure I’m choosing the right surgeon for my needs?
Choosing the right surgeon is arguably the most critical step. I always recommend patients look for board-certified specialists with extensive experience in your specific condition. Resources like finding certified surgeons and reviews of top NJ spine surgeons can guide your decision. Personal consultations should focus on the surgeon’s familiarity with advanced techniques, their approach to patient care, and their success rates. Remember, a surgeon’s expertise in specific procedures like minimally invasive surgery can significantly influence your outcome.
Empowering Your Decision: The Role of Patient Involvement and Second Opinions
Ultimately, your health journey is personal. I encourage my patients to actively participate in their treatment planning, ask questions, and seek second opinions if uncertain. The more informed you are about risks, benefits, and alternative options—such as spinal stenosis surgery details—the better your decision-making process. Sharing your experiences or concerns in comments or with your care team can provide clarity and peace of mind, guiding you toward the best timing for your surgery and recovery plan.
The Nuanced Role of Diagnostic Imaging in Surgical Decision-Making
In my extensive clinical practice, I’ve observed that advanced imaging modalities like functional MRI and dynamic X-rays are increasingly pivotal in determining the precise timing for surgical intervention. These tools go beyond standard MRI, revealing subtle instability or nerve compression that static images might miss. For example, dynamic flexion-extension X-rays can expose spinal instability during movement, guiding us toward timely stabilization procedures. According to a comprehensive review in the Journal of Spinal Disorders & Techniques, integrating these sophisticated imaging techniques enhances our ability to tailor interventions accurately, minimizing unnecessary surgeries and preventing irreversible nerve damage.
How Do Functional Assessments Predict Surgical Outcomes?
Functional assessments, including gait analysis and neurophysiological tests, have become invaluable in my practice for predicting which patients will benefit most from early surgical intervention. These evaluations help identify early signs of neural compromise that aren’t always apparent on imaging alone. For instance, subtle changes in walking patterns or electromyography findings can flag impending neurological deterioration, prompting proactive surgical planning. This proactive approach aligns with recent guidelines emphasizing early intervention when functional decline is evident, ultimately improving long-term prognosis and patient satisfaction.
Can Biomarkers Signal the Optimal Window for Surgery?
Emerging research suggests that specific biomarkers, such as neurofilament light chain levels, could serve as early indicators of nerve injury severity, offering a biochemical window into the progression of degenerative spinal conditions. Although still in experimental stages, these biomarkers hold promise for refining surgical timing, especially in complex cases where clinical and imaging findings are equivocal. A recent study published in Spine highlights how integrating biomarker analysis with traditional assessments might revolutionize personalized surgical planning, ensuring intervention occurs before irreversible damage ensues. As a spine specialist dedicated to personalized care, I advocate for ongoing research and cautious adoption of these innovative tools in clinical practice.
Engage with Your Expert: Deepen Your Understanding of Spinal Surgery Timing
If you’re navigating the complex decision of when to pursue surgery, I invite you to share your experiences or ask questions. Staying informed about cutting-edge diagnostic techniques and understanding their implications can empower you to make timely, evidence-based decisions. For personalized guidance tailored to your unique condition, consider consulting a top-rated NJ spine surgeon—your proactive approach today can safeguard your mobility and quality of life tomorrow. To explore more about advanced diagnostic strategies, visit this resource on spinal decompression.
Things I Wish I Knew Earlier (or You Might Find Surprising)
1. Not Every Pain Requires Surgery
Early in my journey, I believed that surgery was the inevitable solution for severe back pain. However, I discovered that many cases can be managed effectively with non-surgical treatments, and rushing into surgery isn’t always the best move. Understanding this helped me feel more in control of my health decisions.
2. Timing Can Make a Difference
Waiting too long to seek surgical evaluation might lead to irreversible nerve damage, but acting too quickly can expose you to unnecessary risks. I learned that early, personalized assessment by a skilled NJ spine surgeon can be crucial for optimal outcomes.
3. Advanced Imaging Tools Are Game Changers
Modern diagnostic techniques like dynamic X-rays and functional MRI have transformed how we determine the best time for surgery. These tools reveal subtle instabilities or nerve compressions that static images might miss, guiding better decision-making.
4. The Power of a Second Opinion
Getting a second opinion provided me with peace of mind and a clearer understanding of my options. It’s a vital step, especially when facing significant procedures like spinal decompression or fusion.
5. Recovery Can Be Faster Than You Expect
Thanks to minimally invasive techniques available in NJ, recovery times are shorter, and pain relief is quicker. I wish I had known earlier how these innovations could make a big difference in the healing process.
Resources I’ve Come to Trust Over Time
- American Association of Neurological Surgeons: Their website offers comprehensive, evidence-based information on spine conditions and treatments. It’s a reliable resource I often recommend.
- NJ Spine Surgeons Online: The detailed profiles and reviews of top NJ spine surgeons helped me find specialists with the right expertise for my needs.
- Spine Journal: This peer-reviewed journal keeps me updated on the latest research and technological advancements in spinal surgery, ensuring I stay informed about new options.
Parting Thoughts from My Perspective
Deciding when to pursue spine surgery in New Jersey can feel overwhelming, but understanding your body’s signals and trusting expert guidance are key. I’ve learned that early evaluation, the right diagnostic tools, and choosing a skilled surgeon can truly impact your recovery and quality of life. If this resonated with you, I’d love to hear your thoughts. And if you’re considering your options, don’t hesitate to seek a second opinion—your future self will thank you.
,