Strategic Foundations of Post-Surgery Spine Rehabilitation in New Jersey
Post-operative rehabilitation following spine surgery in New Jersey demands a meticulously crafted, evidence-based approach to optimize functional recovery and minimize complications. The multifaceted nature of spine rehab integrates biomechanical restoration, neurophysiological adaptation, and psychosocial support—each element critical to successful outcomes. Understanding the regional nuances in rehabilitation protocols and patient demographics enhances tailored care pathways, leveraging advanced therapeutic modalities available through NJ specialists.
Integrating Advanced Therapeutic Techniques for Enhanced Spine Recovery
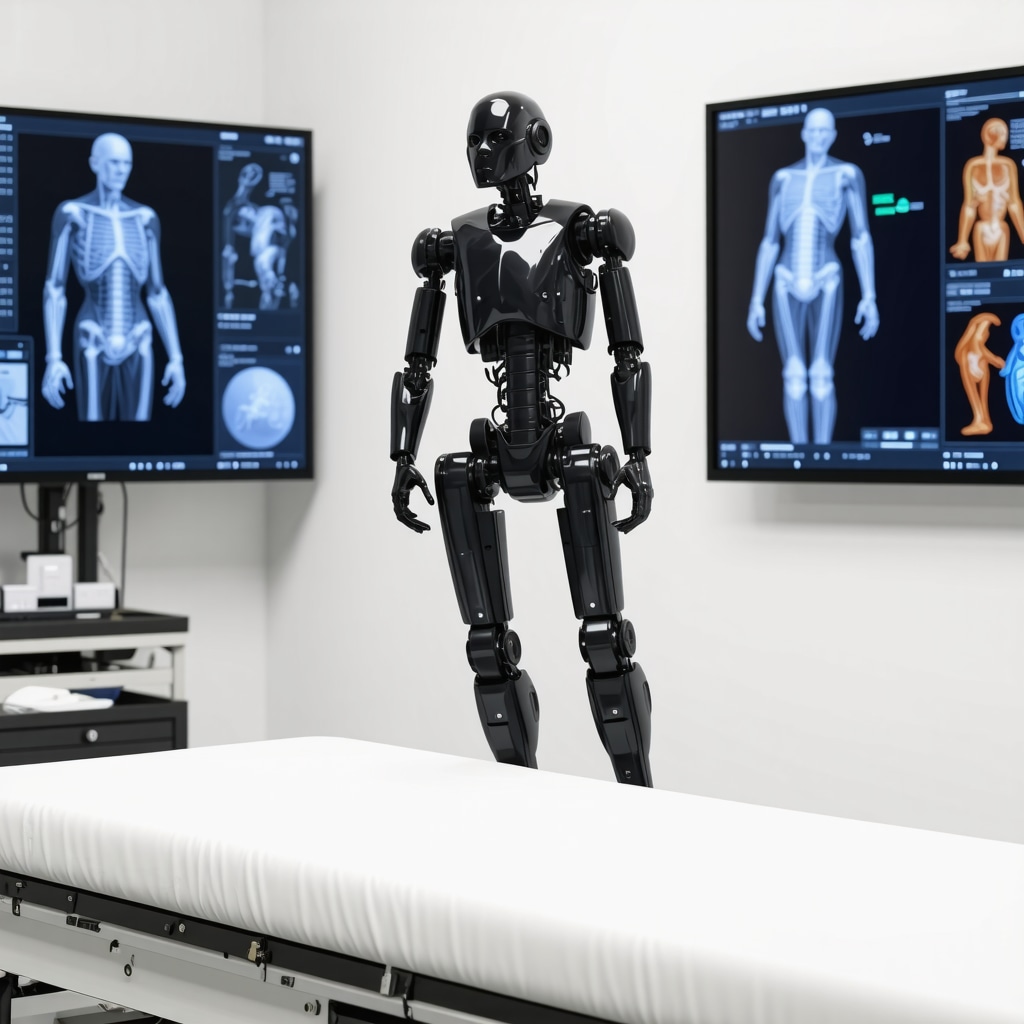
Advanced rehabilitation strategies in NJ capitalize on innovations such as neuromuscular re-education, proprioceptive training, and targeted myofascial release. These methods aim to restore spinal stability and enhance neural integration post-surgery. Incorporating technology-assisted interventions, including robotic-assisted physiotherapy and biofeedback mechanisms, further refines patient outcomes by facilitating precise movement retraining and optimizing muscle activation patterns.
How Do NJ Spine Rehab Protocols Address the Complexities of Post-Surgical Pain and Mobility Limitations?
Addressing post-surgical pain and mobility restrictions in NJ involves a multidisciplinary framework combining pharmacologic management, manual therapy, and tailored exercise regimens. The protocols emphasize gradual load progression and functional restoration while monitoring for signs of complications such as failed back surgery syndrome. Emphasis is placed on individualized patient assessment to balance analgesia with active rehabilitation, ensuring alignment with surgical objectives and minimizing risk of re-injury.
Expert Insights on Nutritional and Psychological Support in Spine Surgery Rehabilitation
Optimizing nutritional status plays a pivotal role in accelerating tissue healing and modulating inflammatory responses post-spine surgery. NJ spine rehab programs incorporate dietary guidance emphasizing anti-inflammatory nutrients and adequate protein intake to support bone and soft tissue repair. Concurrently, psychological resilience is fostered through cognitive-behavioral strategies addressing anxiety, depression, and pain catastrophizing, which are known to influence rehabilitation adherence and outcomes.
Leveraging Local Expertise and Resources for Comprehensive Post-Surgery Care
New Jersey’s network of board-certified spine surgeons and rehabilitation specialists collaborate to provide integrated care pathways. Patients benefit from coordinated interventions, including minimally invasive surgical follow-ups and evidence-based rehab techniques. To explore cutting-edge surgical innovations that complement rehabilitation efforts, consider reviewing top spine surgery techniques to watch in 2025. Moreover, understanding the nuances between orthopedic and neurosurgical spine care can further refine patient-specific rehab planning (orthopedic vs neurosurgeon considerations).
Call to Action: Engage with NJ Spine Rehabilitation Experts for Personalized Recovery Strategies
For patients and clinicians seeking to deepen their understanding of rehabilitation nuances post-spine surgery in NJ, we invite you to explore detailed recovery timelines and expert recovery care tips at after spine surgery recovery care tips from NJ experts. Contribute your experiences or professional insights to foster a community advancing spine rehab excellence.
According to the National Center for Biotechnology Information (NCBI), structured rehabilitation programs significantly improve functional outcomes and reduce chronic pain post-spinal surgery, underscoring the critical role of specialized post-operative care.
Innovative Pain Management Approaches in NJ Spine Rehabilitation
Effective pain control remains a cornerstone of post-spine surgery rehabilitation, directly influencing patients’ ability to engage in therapeutic activities and achieve optimal recovery. New Jersey rehabilitation specialists increasingly adopt multimodal pain management strategies that reduce reliance on opioids, incorporating modalities such as transcutaneous electrical nerve stimulation (TENS), ultrasound therapy, and nonsteroidal anti-inflammatory drugs (NSAIDs) tailored to individual patient profiles. This integrative approach mitigates risks of dependency while enhancing functional restoration.
Customizing Mobility Restoration: Functional Training Beyond Traditional Therapy
Restoring mobility post-surgery extends beyond basic range-of-motion exercises. NJ experts emphasize functional training that aligns rehabilitation with patients’ daily life demands and occupational roles. This includes dynamic balance activities, task-specific movement retraining, and ergonomic education to prevent compensatory patterns that could lead to secondary musculoskeletal issues. Such precision in therapy design fosters sustainable improvements and reduces recurrence of spine-related disabilities.
What Role Does Emerging Technology Play in Transforming Post-Spine Surgery Rehabilitation Outcomes?
Emerging technologies are revolutionizing post-operative spine care by enabling precise, data-driven rehabilitation protocols. Wearable sensors provide real-time feedback on spinal alignment and muscle activation, allowing therapists to adjust interventions dynamically. Virtual reality (VR) platforms create immersive environments for pain distraction and motivation enhancement, while robotic exoskeletons assist in gait training for patients with complex mobility impairments. These innovations collectively accelerate recovery timelines and improve patient engagement, representing a paradigm shift in spine rehabilitation.
For a comprehensive overview of advanced surgical techniques complementing these rehab innovations, visit top spine surgery techniques to watch in 2025.
Psychosocial Integration: Addressing Mental Health in Spine Surgery Recovery
Psychological health critically impacts rehabilitation outcomes. NJ spine rehab programs increasingly embed mental health support within their care continuum, employing screening tools to identify anxiety, depression, and fear-avoidance behaviors early. Cognitive-behavioral therapy (CBT) and mindfulness-based stress reduction (MBSR) techniques help patients develop coping mechanisms, improve pain tolerance, and bolster adherence to physical therapy regimens. This biopsychosocial model underscores the interdependence of mind and body in spine recovery.
Collaborative Care Models: Enhancing Continuity and Patient-Centered Rehabilitation
New Jersey’s spine care landscape benefits from integrated collaborative models that connect surgeons, rehabilitation specialists, primary care providers, and mental health professionals. Such coordination ensures seamless transitions across treatment phases, personalized goal setting, and ongoing patient education. The synergy among these disciplines elevates care quality and reduces fragmentation, fostering a patient-centered approach that adapts to evolving recovery needs.
According to a recent review published in The Spine Journal, multidisciplinary rehabilitation programs yield superior functional outcomes and quality of life improvements compared to conventional approaches, reinforcing the value of integrative care.
Engage with NJ Experts to Elevate Your Spine Surgery Recovery Journey
We encourage patients and healthcare professionals to share their perspectives and questions on advanced spine rehabilitation strategies. Your participation enriches the collective knowledge and supports continuous improvement in care standards. Explore additional expert insights on optimizing recovery at after spine surgery recovery care tips from NJ experts and join the conversation.

Harnessing Biomechanical Modeling to Personalize Post-Spine Surgery Rehabilitation
Advanced biomechanical modeling techniques are transforming the customization of rehabilitation protocols in New Jersey. By utilizing patient-specific imaging data and computational analysis, clinicians can simulate spinal load distribution and predict tissue stress during various activities. This granular insight enables the design of exercise regimens that precisely target vulnerable regions while promoting optimal spinal alignment and function. Such personalized approaches mitigate the risk of re-injury and expedite the restoration of complex motor patterns essential for daily activities and occupational demands.
What Are the Latest Developments in Biomechanical Modeling That Enhance Spine Rehab Outcomes?
Recent innovations include the integration of finite element analysis (FEA) with real-time movement capture, allowing continuous feedback on biomechanical parameters during therapy sessions. This hybrid methodology facilitates dynamic adjustments to rehabilitation exercises based on instantaneous patient performance and tolerance. Furthermore, machine learning algorithms analyze longitudinal patient data to refine predictive models, improving prognostic accuracy for functional recovery timelines. These advancements underscore a shift from static to adaptive rehabilitation frameworks that accommodate individual variability in healing trajectories.
Neuroplasticity-Driven Rehabilitation: Maximizing Neural Recovery Post-Spinal Surgery
Emerging evidence highlights neuroplasticity as a pivotal mechanism underlying successful post-surgical rehabilitation. New Jersey specialists incorporate interventions such as task-specific repetitive training, mirror therapy, and sensory stimulation to promote cortical reorganization and neural pathway reinforcement. By engaging central nervous system adaptability, these methods enhance motor control and reduce maladaptive compensations. Combining neuroplasticity-focused strategies with conventional physical therapy accelerates functional integration and improves long-term outcomes, especially in patients with complex neurological deficits.
Integrating Precision Medicine: Genetic and Biomarker Profiling in Rehabilitation Planning
The advent of precision medicine is beginning to influence spine surgery rehabilitation by informing individualized care based on genetic and biomarker profiles. In New Jersey, select centers are pioneering the use of inflammatory cytokine profiling and genetic markers associated with connective tissue repair capacity to tailor post-operative protocols. This approach enables clinicians to predict patients’ healing potential and susceptibility to complications such as fibrosis or chronic pain syndromes. Consequently, rehabilitation intensity and adjunctive therapies can be modulated to optimize tissue recovery and functional restoration.
Collaborative Robotics and Artificial Intelligence: The Future of NJ Spine Therapy
The integration of robotics and artificial intelligence (AI) in rehabilitation represents a frontier in enhancing precision and efficacy of post-spine surgery care. Robotic exoskeletons assist in guided movement repetitions with adjustable assistance levels, fostering neuromuscular re-education while minimizing patient fatigue. AI-driven platforms analyze performance metrics to customize therapy parameters dynamically, ensuring progressive challenge without overexertion. These technologies are particularly beneficial for patients with complex comorbidities or delayed recovery phases, offering scalable, consistent interventions that augment human therapist expertise.
According to a 2023 study published in Neurorehabilitation and Neural Repair, the application of AI-assisted robotics significantly improved gait symmetry and reduced pain scores in post-lumbar surgery patients, illustrating the transformative potential of these modalities.
Call to Action: Collaborate with NJ Spine Rehabilitation Experts to Explore Cutting-Edge Recovery Solutions
To harness these advanced methodologies and technologies for optimal spine surgery recovery, engage with New Jersey’s leading rehabilitation specialists. Delve deeper into personalized rehab strategies and technological innovations by visiting after spine surgery recovery care tips from NJ experts. Join the community dedicated to pioneering evidence-based, patient-centric spine rehabilitation.
Precision Biomechanics: Revolutionizing Personalized Rehabilitation Protocols
The evolution of biomechanical modeling in New Jersey’s post-spine surgery rehabilitation landscape offers unprecedented precision in tailoring recovery regimens. Utilizing patient-specific finite element analysis (FEA) integrated with dynamic motion capture, clinicians can now simulate in vivo spinal load distributions during functional activities. This approach transcends traditional static assessments, enabling adaptive exercise prescriptions that mitigate localized tissue stress and optimize spinal kinematics, thereby reducing the risk of recurrent injury.
Which cutting-edge biomechanical tools are redefining spine rehab personalization?
Emerging platforms incorporate machine learning algorithms that analyze longitudinal biomechanical and clinical data, refining predictive models for recovery trajectories. Instruments such as wearable inertial measurement units (IMUs) provide continuous real-time feedback on posture and spinal alignment, facilitating immediate therapeutic adjustments. These innovations collectively empower clinicians to design nuanced, patient-centric interventions that accommodate individual variability in healing and functional demands.
Neuroplasticity-Driven Strategies: Enhancing Functional Neural Recovery
Neurorehabilitative techniques targeting cortical reorganization are gaining traction among NJ specialists. Task-specific repetitive training, paired with adjunctive sensory modalities like mirror therapy and transcranial magnetic stimulation (TMS), stimulate neuroplastic adaptations critical for restoring motor control. By engaging these central nervous system mechanisms, therapists foster improved synaptic efficacy and neural pathway remapping, which are essential for overcoming post-surgical motor deficits and preventing maladaptive compensations.
Integrating Precision Medicine: Genetic and Biomarker-Guided Rehabilitation Customization
Advancements in genomics and biomarker profiling enable NJ clinicians to stratify patients based on their inherent tissue repair capacities and inflammatory responses. Genetic markers linked to collagen synthesis and cytokine profiles inform rehabilitation intensity and adjunct therapies, optimizing healing while minimizing fibrosis and chronic pain development. This precision medicine paradigm represents a transformative leap toward truly individualized spine surgery recovery plans.
Artificial Intelligence and Robotics: Catalyzing a New Era of Rehabilitation Efficiency
The integration of AI-driven analytics with robotic-assisted therapy systems is redefining therapeutic delivery in New Jersey. Robotic exoskeletons provide precisely calibrated support and resistance, facilitating high-repetition, task-specific motor training that enhances neuromuscular re-education. Concurrently, AI algorithms analyze patient performance metrics to dynamically adjust therapy parameters, ensuring optimal challenge without overexertion. This synergy accelerates functional gains and broadens accessibility for patients with complex impairments.
Notably, a 2023 publication in Neurorehabilitation and Neural Repair documented significant improvements in gait symmetry and pain reduction among post-lumbar surgery patients utilizing AI-assisted robotics, emphasizing the clinical efficacy of these modalities.
Psychosocial Integration: Advanced Cognitive-Behavioral Interventions in NJ Rehab Programs
Recognizing the intricate biopsychosocial interplay in spine recovery, New Jersey rehabilitation frameworks increasingly embed sophisticated behavioral interventions. Cognitive-behavioral therapy (CBT) modules tailored to pain catastrophizing and kinesiophobia, coupled with mindfulness-based stress reduction (MBSR), enhance patient adherence and psychological resilience. Early identification of mental health variables via validated screening tools enables proactive integration of psychological support, optimizing functional rehabilitation outcomes.
Collaborative Multidisciplinary Models: Streamlining Continuity of Care
The convergence of orthopedic surgeons, neurosurgeons, physical therapists, pain specialists, and mental health professionals epitomizes New Jersey’s commitment to integrated spine care. This multidisciplinary synergy facilitates cohesive rehabilitation pathways, personalized goal-setting, and adaptive treatment modifications responsive to patient progress and emerging clinical indicators. Such models are substantiated by evidence from The Spine Journal, which affirms superior functional and quality of life outcomes arising from coordinated care frameworks.
Call to Action: Collaborate with New Jersey’s Spine Rehabilitation Pioneers to Unlock Cutting-Edge Recovery Potential
Engage with leading NJ spine rehabilitation experts to explore these advanced, technology-infused methodologies that redefine post-surgical recovery. Visit after spine surgery recovery care tips from NJ experts to deepen your understanding and participate in a progressive community dedicated to elevating rehabilitation standards through evidence-based innovation.

Expert Insights & Advanced Considerations
Integrating Real-Time Biomechanical Feedback for Tailored Rehab
Leveraging wearable sensors and finite element analysis enables clinicians to monitor spinal load and alignment dynamically, allowing immediate modification of rehabilitation exercises. This precision reduces risks of re-injury and accelerates functional recovery by ensuring exercises remain within patient-specific biomechanical thresholds.
Harnessing Neuroplasticity-Driven Modalities to Optimize Motor Recovery
Incorporating task-specific repetitive training, mirror therapy, and sensory stimulation engages cortical reorganization mechanisms. This neuroplasticity-focused approach enhances motor control restoration and mitigates maladaptive compensations, particularly vital for patients with neurological impairments following spine surgery.
Employing Precision Medicine to Customize Rehabilitation Intensity
Utilizing genetic and inflammatory biomarker profiles allows for stratification of patients’ healing capacities. Tailoring rehabilitation protocols based on these profiles improves tissue repair outcomes and minimizes chronic pain risks, representing a significant advancement in individualized post-operative care.
Integrating Robotics and AI for Enhanced Rehabilitation Efficiency
Robotic exoskeletons combined with AI-driven performance analytics facilitate high-repetition, task-specific motor training with dynamic difficulty adjustment. This synergy maximizes neuromuscular re-education effectiveness while minimizing patient fatigue, improving recovery trajectories in complex cases.
Embedding Psychosocial Interventions to Support Holistic Recovery
Advanced cognitive-behavioral therapies and mindfulness-based stress reduction integrated into rehabilitation programs address psychological barriers such as pain catastrophizing and fear-avoidance. Early mental health screening ensures timely psychosocial support, enhancing adherence and overall functional outcomes.
Curated Expert Resources
The Spine Journal: A premier peer-reviewed publication offering comprehensive reviews on multidisciplinary rehabilitation models and their superior outcomes, critical for understanding integrative care effectiveness.
National Center for Biotechnology Information (NCBI): Provides access to extensive research on structured rehabilitation programs and evidence-based pain management strategies post-spinal surgery.
Neurorehabilitation and Neural Repair: A specialized journal presenting cutting-edge studies on robotics and AI applications in spine rehabilitation, essential for clinicians aiming to adopt innovative technologies.
New Jersey Spine Surgeons Online: This platform hosts detailed guides and expert insights on surgical techniques, rehabilitation protocols, and patient-centered care pathways tailored to New Jersey’s unique healthcare landscape.
American Physical Therapy Association (APTA): Offers advanced resources on neuroplasticity and functional training methodologies that complement spine surgery recovery.
Final Expert Perspective
The evolving landscape of post-surgery spine rehabilitation in New Jersey embodies a sophisticated convergence of biomechanical precision, neuroplasticity-driven strategies, precision medicine, and cutting-edge technology integration. These advancements underscore a paradigm shift towards highly individualized, multidisciplinary care that holistically addresses physical and psychosocial dimensions of recovery. Embracing this comprehensive approach not only optimizes functional outcomes but also elevates patient quality of life.
For those committed to advancing their understanding or seeking personalized recovery solutions, engaging with NJ’s leading spine rehabilitation experts and exploring detailed resources such as after spine surgery recovery care tips from NJ experts can provide invaluable guidance. We encourage healthcare professionals and patients alike to contribute their insights and experiences, fostering a collaborative environment dedicated to excellence in spine rehabilitation.
