Comprehensive Insights into Spinal Decompression Surgery in Union County, NJ
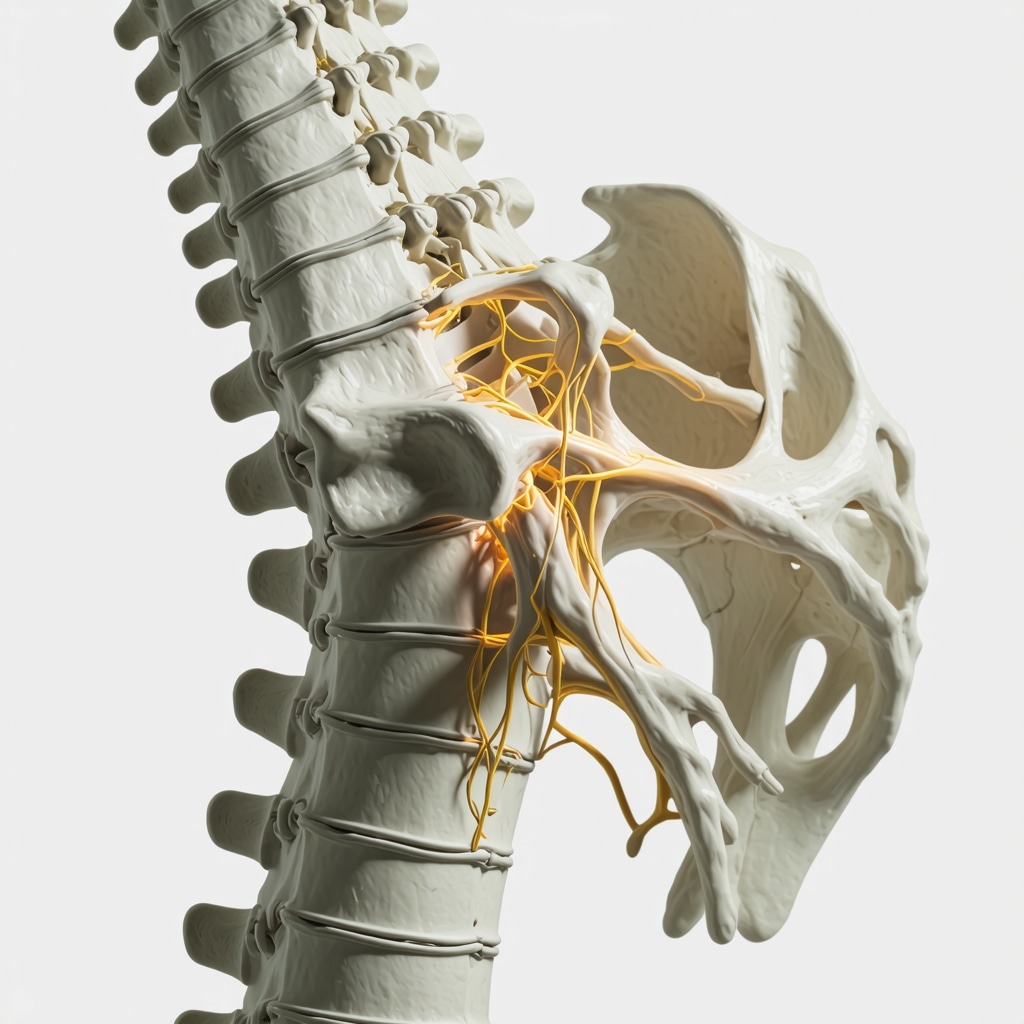
Spinal decompression surgery represents a pivotal intervention for patients suffering from debilitating spinal nerve compression, particularly in regions like Union County, NJ, where advanced spine care is accessible yet demands nuanced understanding. This procedure addresses pathologies such as herniated discs, spinal stenosis, and degenerative disc disease that contribute to chronic pain and neurological deficits. Navigating this complex surgical landscape requires a foundation of expert knowledge about indications, technological advances, patient selection, and expected outcomes.
Advanced Surgical Techniques and Their Impact on Patient Outcomes
The evolution of spinal decompression has been marked by the integration of minimally invasive methods, enhancing precision while reducing tissue disruption. Techniques such as microdiscectomy and endoscopic decompression optimize neural element relief with diminished recovery time, aligning with patient-centric goals. Union County’s spine specialists increasingly adopt these approaches, leveraging intraoperative imaging and neuro-monitoring to mitigate risks. Understanding these modalities is essential for patients evaluating surgical options and for providers aiming to tailor interventions based on individual pathology and anatomy.
How Do Patient-Specific Factors Influence Surgical Approach Selection in Union County?
Patient heterogeneity necessitates personalized surgical planning. Factors including age, comorbidities, anatomical variations, and previous spine interventions critically influence the choice between open versus minimally invasive decompression. For example, elderly patients with osteoporosis might benefit from less invasive approaches to minimize perioperative complications, whereas complex multilevel stenosis may require open decompression with fusion. Union County surgeons conduct comprehensive preoperative assessments, incorporating advanced imaging and functional evaluations, to optimize surgical strategy and prognosis.
Interdisciplinary Collaboration and Postoperative Rehabilitation Paradigms
Effective spinal decompression outcomes hinge not only on surgical skill but also on coordinated postoperative rehabilitation. Integration between orthopedic surgeons, neurosurgeons, physiotherapists, and pain specialists forms a continuum of care that enhances functional recovery and reduces recurrence risk. In Union County, tailored rehabilitation protocols are implemented early to restore mobility, strengthen paraspinal musculature, and manage pain. This multidisciplinary approach reflects evidence-based practices documented in journals like “The Spine Journal,” underscoring the importance of comprehensive care beyond the operating room (Spine Journal, 2020).
Expert Resources to Deepen Your Understanding of Spine Surgery in New Jersey
To navigate the complexities of spinal decompression surgery effectively, patients and clinicians alike should consult authoritative resources such as Understanding Spinal Decompression Surgery in 2025 which provides cutting-edge insights tailored to NJ populations. This cornerstone content elucidates procedural nuances, risk-benefit analyses, and emerging technological trends relevant to Union County residents.
Engage with the Community of Experts and Expand Your Spine Care Knowledge
Are you a patient or professional seeking to contribute to or learn from advanced spine care discourse? Explore our extensive collection of expert-level articles and case studies at NJ Spine Surgeons Contact. Sharing clinical experiences and questions fosters a richer understanding of spinal decompression and elevates community health outcomes.
Personalized Surgical Innovations: Tailoring Decompression to Unique Patient Profiles
In the realm of spinal decompression surgery, the paradigm has shifted from a one-size-fits-all approach to a highly individualized treatment plan. Surgeons in Union County now integrate genomic data, advanced imaging, and biomechanical assessments to predict patient-specific responses to various decompression techniques. This precision medicine angle not only informs the selection between microdiscectomy, endoscopic decompression, or open surgery but also anticipates postoperative recovery trajectories, enabling proactive rehabilitation planning.
Robotic-Assisted Technologies Enhancing Surgical Precision and Safety
Robotic-assisted spine surgery has emerged as a transformative tool in complex decompression procedures. These systems provide enhanced 3D visualization and tremor filtration, which significantly improve the accuracy of nerve decompression and implant placements. Union County centers adopting these technologies report reduced operative times, minimized blood loss, and lower complication rates, which collectively optimize patient outcomes and satisfaction. For a detailed overview of these advancements, see our Robotic Assisted Spine Surgery resource.
What Are the Ethical Considerations When Implementing Cutting-Edge Spine Surgery Technologies?
The integration of novel surgical technologies raises important ethical questions surrounding equitable access, informed consent, and long-term data transparency. While robotic-assisted procedures promise superior outcomes, they also entail higher costs and require specialized training, potentially limiting availability to certain populations. Surgeons and healthcare policymakers in Union County must navigate these challenges by balancing innovation with inclusivity, ensuring patients receive comprehensive information about risks, benefits, and alternatives.
Holistic Postoperative Strategies: Beyond Surgery to Sustainable Recovery
Postoperative care in spinal decompression transcends immediate wound healing, encompassing multidisciplinary strategies for sustained functional improvement. Incorporating cognitive-behavioral therapy, nutritional optimization, and personalized physical therapy protocols fosters resilience against chronic pain and disability. Recent studies underscore the pivotal role of patient education and mental health support in enhancing adherence to rehabilitation, ultimately reducing the incidence of failed back surgery syndrome (National Institutes of Health, 2019). Union County practices increasingly integrate these dimensions, reflecting a holistic care model.
For practitioners and patients eager to deepen their understanding of spinal surgery advances and recovery, we invite you to explore our extensive expert content, including detailed discussions on Minimally Invasive Spine Surgery Benefits and Effective Spine Rehab Processes. Sharing your experiences or posing questions in the comments can enrich the community discourse and support others facing similar challenges.
Integrating Advanced Biomechanical Modeling to Optimize Spinal Decompression Outcomes
The incorporation of biomechanical modeling into surgical planning represents a frontier in personalized spinal decompression surgery. Utilizing finite element analysis (FEA), surgeons in Union County are now able to simulate the mechanical behavior of spinal segments under various decompression scenarios. This allows for precise prediction of stress distribution and potential instability post-procedure, enabling preemptive strategies such as targeted fusion or reinforcement. By marrying patient-specific imaging data with biomechanical simulations, surgical teams can tailor interventions that maximize neural decompression while preserving spinal integrity.
These computational models often incorporate variables like bone density, disc degeneration grade, and facet joint morphology, providing a multi-dimensional perspective that transcends traditional imaging assessments. The result is a clinically actionable roadmap that enhances decision-making and reduces postoperative complications.
How Does Artificial Intelligence Enhance Preoperative Planning and Risk Stratification in Spinal Decompression?
Artificial intelligence (AI) and machine learning algorithms have begun to revolutionize preoperative evaluation by analyzing vast datasets of patient characteristics, imaging findings, and surgical outcomes. In Union County, AI-powered platforms assist surgeons by predicting individualized risks such as infection, neurologic deficits, and recovery duration. These tools continuously learn from local and global data, refining their predictive accuracy over time.
Moreover, AI aids in automated image segmentation and anomaly detection, expediting diagnostic workflows. This fusion of AI with clinical expertise not only improves surgical precision but also facilitates shared decision-making with patients through transparent risk communication.
Exploring the Role of Neurophysiological Monitoring Innovations During Complex Decompression Procedures
Intraoperative neurophysiological monitoring (IONM) has become indispensable in safeguarding neural structures during spinal decompression. Recent technological advances include high-density electromyography and real-time somatosensory evoked potentials with enhanced signal fidelity. Union County surgical centers integrate multimodal IONM to detect subtle changes in nerve function instantaneously, permitting immediate corrective action.
The challenge lies in interpreting complex neurophysiological data amidst the dynamic surgical milieu. Expert neurophysiologists collaborate closely with surgeons to contextualize alerts, differentiating between transient disturbances and significant neural compromise. This synergy reduces the incidences of postoperative neurological deficits and supports aggressive yet safe decompression strategies.
Leveraging Regenerative Medicine Adjuncts to Promote Disc and Nerve Healing Post-Decompression
Emerging regenerative therapies offer promising adjuncts to traditional decompression surgery. Techniques such as platelet-rich plasma (PRP) injections and stem cell therapies are being investigated to enhance disc regeneration and nerve repair after surgical intervention. Union County clinics engaged in clinical trials are pioneering protocols that integrate these biologics with decompression, aiming to improve long-term functional outcomes and delay degenerative progression.
These interventions seek to modulate the local microenvironment, attenuating inflammation and promoting cellular proliferation. While still investigational, early data suggest potential reductions in postoperative pain and faster functional recovery, heralding a paradigm shift towards biologically augmented spine surgery.
What Are the Challenges and Opportunities in Implementing Regenerative Medicine in Spine Surgery?
Despite encouraging progress, regenerative medicine faces hurdles including variability in product preparation, regulatory constraints, and cost-effectiveness considerations. The heterogeneity of spinal pathologies further complicates patient selection and outcome standardization. Union County experts advocate for rigorous clinical trials and multidisciplinary collaboration to validate these approaches before widespread adoption.
Continued innovation and evidence generation will be critical to integrate regenerative adjuncts effectively within the spinal decompression treatment algorithm.
For clinicians and patients intrigued by these cutting-edge developments, we encourage exploring detailed resources and engaging with Union County’s spine surgery experts through our NJ Spine Surgeons Contact platform. Sharing insights and experiences fosters advancement in this rapidly evolving domain.
Harnessing Artificial Intelligence for Revolutionary Preoperative Insights
Artificial intelligence (AI) is fundamentally transforming preoperative planning in spinal decompression surgery within Union County’s advanced medical centers. By leveraging sophisticated machine learning algorithms that analyze comprehensive datasets—ranging from patient demographics and comorbidities to high-resolution imaging and historical surgical outcomes—clinicians can now stratify risks with unprecedented precision. This predictive analytics capability not only forecasts potential complications such as infection rates, nerve injury, or delayed recovery but also informs surgical approach tailoring, optimizing patient-specific strategies.
Biomechanical Modeling: The New Frontier in Personalized Spine Surgery
Building upon traditional imaging, the integration of finite element analysis (FEA) and other biomechanical modeling techniques allows surgeons to simulate spinal load distributions post-decompression. This proactive evaluation facilitates identification of segments susceptible to instability or accelerated degeneration, thus enabling preemptive incorporation of stabilizing procedures or reinforcement techniques. Such data-driven insights significantly reduce the risk of postoperative complications and enhance long-term surgical success.
How Are Emerging Neurophysiological Monitoring Technologies Improving Intraoperative Safety During Complex Decompression Procedures?
Recent innovations in intraoperative neurophysiological monitoring (IONM) have introduced high-density electromyography and real-time somatosensory evoked potential mapping, offering heightened sensitivity to neural function fluctuations. These modalities provide instantaneous feedback, allowing surgical teams in Union County to detect and address nerve compromise immediately. The integration of multimodal IONM frameworks, supported by expert neurophysiologists, advances the precision and safety of decompression surgeries, especially in anatomically complex or revision cases.
Regenerative Medicine Adjuncts: Catalyzing Disc and Neural Repair Post-Surgery
Emerging biologic therapies, including platelet-rich plasma (PRP) and mesenchymal stem cell injections, are being explored as adjuncts to conventional decompression procedures to enhance endogenous healing processes. Experimental protocols at select Union County centers aim to modulate inflammatory cascades and stimulate cellular regeneration within intervertebral discs and compressed neural elements. While still under rigorous clinical evaluation, early evidence suggests these regenerative approaches may reduce postoperative pain, accelerate functional recovery, and potentially delay degenerative progression.
Ethical and Practical Challenges in Implementing Advanced Spine Surgery Technologies
Despite the promise of robotic-assisted surgery, AI-driven analytics, and regenerative medicine, ethical considerations such as equitable access, cost transparency, and informed consent remain paramount. Union County healthcare providers and policymakers actively engage in dialogues to address disparities that may arise from technology adoption, ensuring that innovations complement rather than complicate patient-centered care.
For authoritative perspectives on the integration of these advanced modalities, consult the latest research in The Journal of Spine Surgery (2020), which provides comprehensive analyses of AI and regenerative medicine applications in spine surgery.
Discover How Cutting-Edge Innovations Can Transform Your Spine Care Journey
To explore how these advanced technologies and strategies can enhance your treatment outcomes or clinical practice, engage with Union County’s leading spine surgery experts through our NJ Spine Surgeons Contact platform. Share your case details or inquire about the latest procedural advancements to receive personalized guidance grounded in the forefront of spinal decompression surgery.
Expert Insights & Advanced Considerations
Personalized Surgical Planning: The Imperative of Integrating Multimodal Data
In Union County, NJ, spinal decompression surgery outcomes are substantially enhanced when surgical plans synthesize genomic information, biomechanical modeling, and comprehensive imaging. This multifaceted data integration enables surgeons to tailor decompression techniques—whether minimally invasive microdiscectomy or more extensive open surgery—with precision that anticipates patient-specific anatomical and physiological responses, optimizing recovery and minimizing complications.
Robotic-Assisted Surgery: Balancing Innovation with Ethical Responsibility
The adoption of robotic-assisted technologies in spinal decompression has revolutionized surgical accuracy and safety. However, experts emphasize the necessity of ensuring equitable access and transparent patient consent given the cost and training requirements. Union County’s spine centers are pioneering frameworks to responsibly implement these tools while maintaining patient-centered care and addressing disparities.
Neurophysiological Monitoring: Critical Safeguards in Complex Procedures
Advanced intraoperative neurophysiological monitoring (IONM) modalities, such as high-density electromyography and real-time somatosensory evoked potentials, have become indispensable for protecting neural integrity during decompression surgeries. The dynamic collaboration between neurophysiologists and surgeons in Union County facilitates immediate response to neural distress signals, thereby reducing postoperative deficits and enabling more assertive decompression when clinically indicated.
Regenerative Medicine Adjuncts: Emerging Frontiers and Clinical Challenges
Biologic therapies like platelet-rich plasma and stem cell injections show promise as adjuncts to spinal decompression by promoting disc and nerve healing. Despite promising early outcomes, rigorous clinical trials and standardized protocols remain essential to address variability and validate long-term benefits in Union County’s advanced spine care landscape.
Curated Expert Resources
Understanding Spinal Decompression Surgery in 2025: A foundational resource that delineates procedural innovations, patient selection nuances, and outcome expectations tailored for New Jersey populations. Explore this guide for comprehensive insights.
Robotic Assisted Spine Surgery: An in-depth analysis of robotic technologies’ impact on surgical precision, safety, and ethical considerations within spine surgery. Learn more here.
Effective Spine Rehab Processes Post Surgery in New Jersey: Evidence-based rehabilitation protocols critical for sustainable recovery following spinal decompression. This resource provides expert recommendations on multidisciplinary care integration. Access detailed guidance.
How Artificial Intelligence Enhances NJ Patient Outcomes: A forward-looking exploration of AI-driven risk stratification and preoperative planning that is transforming spine surgery practices. Discover AI’s role.
Choosing Between Orthopedic and Neurosurgeon for Spine Care: Essential considerations to identify the most appropriate specialist for complex spinal decompression needs. Find out more.
Final Expert Perspective
The landscape of spinal decompression surgery in Union County, NJ, is evolving rapidly through integration of personalized data, robotic assistance, advanced monitoring, and regenerative adjuncts. These innovations collectively empower surgical teams to deliver nuanced, patient-centered care that improves functional outcomes and mitigates risks. However, the ethical imperative to balance technological advancement with equitable access and informed consent remains paramount. For patients and clinicians committed to navigating this complexity, engaging with authoritative resources and expert networks is essential. We encourage you to deepen your exploration of spinal decompression surgery by connecting with Union County’s top specialists via our NJ Spine Surgeons Contact platform. By sharing knowledge and experiences, you contribute to advancing excellence in spine care for the community and beyond.

The article offers an excellent overview of spinal decompression surgery and highlights how personalized approaches in Union County are key to effective treatment. What’s particularly interesting to me is the use of advanced biomechanical modeling to tailor surgery plans — this seems like a game changer in predicting and preventing post-op complications related to spinal instability. From what I understand, integrating genomic data and AI-driven risk assessments can further refine patient selection and recovery strategies, which must greatly benefit patients with complex or multiple spine issues. However, I wonder how accessible these cutting-edge techniques are across different hospitals and to patients of varying socioeconomic backgrounds. Advanced technologies like robotic-assisted surgery and regenerative adjuncts sound promising but might also raise concerns about cost and equity. Given the collaborative rehabilitation approach mentioned, I also think involving patients early in comprehensive recovery plans that address physical and mental health is crucial. I’d love to hear from others who have undergone spinal decompression in Union County: how much did your surgical team tailor the approach based on your specific conditions, and what post-op therapies made the biggest difference in your recovery? Are there challenges you’ve encountered in accessing or coordinating care with these multidisciplinary teams?
This post offers a detailed glimpse into the future of spinal decompression in Union County, highlighting how innovative techniques like biomechanical modeling and AI are transforming patient outcomes. I’ve noticed that many patients, including myself, often worry about the recovery process and how personalized approaches can make a real difference. For instance, understanding preoperative risks through AI-driven risk stratification could help us prepare more effectively and set realistic expectations. The integration of regenerative medicine also seems promising, especially for long-term healing, although I am curious about how widespread access to these treatments is. The mention of robotic-assisted surgery is particularly interesting, as it shows how precision can directly impact safety and success rates. However, I wonder—what are the main barriers for patients to access these advanced options? Can smaller hospitals in the area keep up with such rapid technological innovations, or is there a risk of creating disparities? Overall, it’s exciting to see how multidisciplinary collaboration and technological advancements are shaping a safer, more effective future for spine care.