My Journey into Spinal Surgery: Exploring ALIF & TLIF
Several years ago, I found myself grappling with persistent back pain that no over-the-counter remedies could alleviate. After consulting with my trusted spine specialist, I learned about advanced surgical options like Anterior Lumbar Interbody Fusion (ALIF) and Transforaminal Lumbar Interbody Fusion (TLIF). Sharing my personal experiences and insights, I hope to shed light on these procedures and help others navigate their own journeys.
Decoding ALIF & TLIF: What Are They and How Do They Differ?
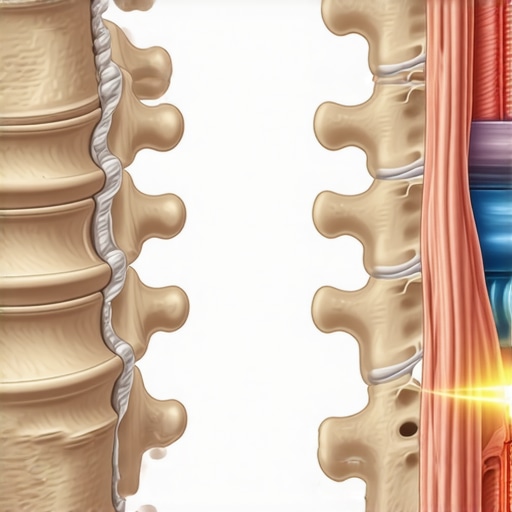
As I delved deeper, I discovered that ALIF involves accessing the spine from the front of the body, allowing for a direct approach to the disc space. In contrast, TLIF approaches the spine from the side or back, which can be beneficial depending on the specific spinal condition. Understanding these differences was crucial in my decision-making process, especially after reviewing authoritative sources like spinal decompression surgery insights.
Pros and Cons: Personal Reflections on Surgical Choices
Is One Approach Clearly Better Than the Other?
From my experience and research, ALIF offers the advantage of preserving back muscles and potentially faster fusion times, but it requires navigating around major blood vessels. TLIF, while more familiar to many surgeons, involves more muscle disruption but can be performed with minimally invasive techniques. My surgeon explained that the choice depends heavily on individual anatomy and specific spinal issues.
According to spine experts, both procedures have high success rates, but they also carry risks such as nerve injury or infection. To ensure I made an informed choice, I explored reputable clinics and verified surgeon credentials, as recommended in guides like finding a qualified spine surgeon.
What Does Recovery Really Look Like?
Recovery was a significant concern for me. I learned that typically, patients may experience relief within weeks, but full fusion can take 6-12 months. During this period, I adhered strictly to my surgeon’s post-operative care instructions and incorporated nutrition tips from trusted sources to support healing, such as eating protein-rich foods and staying hydrated.
One thing I wish I knew earlier: the importance of gentle movement and physical therapy in recovery. I found that early mobilization, under professional guidance, greatly improved my outcomes and reduced discomfort.
How Do I Manage Expectations and Minimize Risks?
It’s natural to worry about potential complications. I discussed extensively with my surgeon about the risks and benefits, and I appreciated the clarity provided in comprehensive guides like spine surgery expectations. Staying informed and choosing a board-certified surgeon were key steps in building trust and confidence in my surgical journey.
If you’re considering ALIF or TLIF, I highly recommend consulting with experienced specialists who use the latest techniques, such as robotic-assisted surgery, which has shown promising outcomes in recent studies. For personalized guidance, don’t hesitate to reach out via contact us.
Have you had similar experiences or questions about spinal fusion procedures? Feel free to share your thoughts or ask for advice below. Your journey deserves personalized care and expert insight!
Exploring the Critical Factors in Choosing the Right Spinal Fusion Technique
When it comes to spinal fusion, understanding the subtle differences between procedures like Anterior Lumbar Interbody Fusion (ALIF) and Transforaminal Lumbar Interbody Fusion (TLIF) is crucial for making informed decisions. Both techniques aim to stabilize the spine and alleviate pain, but their approaches, risks, and recovery profiles vary significantly.
How Do Anatomical Considerations Influence Surgical Approach?
One of the key factors influencing the choice between ALIF and TLIF is the patient’s unique anatomy. ALIF involves accessing the spine from the front through the abdomen, providing a direct view of the disc space and allowing for larger grafts, which can promote faster fusion. However, this approach requires navigating around major blood vessels, increasing the risk of vascular injury. Conversely, TLIF approaches the spine from the back or side, often with minimally invasive techniques that reduce muscle disruption but may involve more limited graft placement.
Experts emphasize that thorough preoperative imaging and assessment are essential to determine which approach aligns best with the patient’s specific spinal pathology. For instance, patients with significant vascular anomalies or prior abdominal surgeries might be better suited for TLIF. Conversely, those needing extensive disc removal and fusion might benefit from the ALIF approach.
What Are the Practical Implications for Recovery and Long-Term Outcomes?
Recovery timelines and success rates are influenced by the surgical technique chosen. ALIF tends to offer quicker initial recovery due to less muscle disruption, but it demands meticulous intraoperative navigation to avoid vascular complications. TLIF, especially when performed minimally invasively, can result in less postoperative pain and quicker mobilization, yet some patients may require longer to achieve full fusion.
Recent studies, such as those summarized in the comprehensive guide on spinal fusion, suggest that both procedures have high success rates when performed by experienced surgeons. Nonetheless, potential risks like nerve injury, infection, or hardware failure remain considerations that should be discussed thoroughly with your surgical team.
How Can You Maximize Your Surgical Outcomes and Minimize Risks?
Preparation is key. Verifying your surgeon’s credentials and their familiarity with the latest minimally invasive and robotic-assisted techniques can significantly impact your recovery trajectory. For example, robotic-assisted spine surgery, explored in detail here, offers enhanced precision and potentially better outcomes.
Additionally, adopting a proactive approach to post-operative care, including proper nutrition, physical therapy, and adherence to activity restrictions, can make a difference. I recommend consulting resources on post-surgical recovery, such as post-operative care tips, to optimize your healing process.
Have You Considered the Long-Term Implications of Fusion Surgery?
Understanding how fusion impacts spinal mobility and the potential for adjacent segment disease is vital. While fusion provides stability, it may alter biomechanics and lead to degeneration of neighboring discs over time. Discussing these factors with your surgeon and exploring alternative or adjunct treatments, such as disc replacement or motion-preserving technologies, can help tailor a personalized treatment plan.
If you’re seeking expert guidance, visiting a top-rated NJ spine surgeon or exploring tips for finding qualified surgeons can ensure you receive care from experienced professionals committed to the latest advancements.
Have questions or want to share your experience with spinal fusion? Drop a comment below or reach out through our contact page. Your insights can help others navigate their own journey to recovery.
Unraveling the Subtleties of Spinal Fusion: A Personal Reflection on Precision and Patient-Centered Care
As I continued my journey through the intricate landscape of spinal surgery, I realized that beneath the broad strokes of procedures like ALIF and TLIF lies a world of nuanced decision-making. Every patient presents a unique puzzle—anatomy, lifestyle, and expectations intertwine to influence the optimal surgical approach. My firsthand experience has shown me that successful outcomes hinge not just on choosing the right technique but on the surgeon’s ability to personalize each step.
What Are the Hidden Complexities in Preoperative Planning?
One aspect I’d like to highlight, based on my research and conversations with seasoned surgeons, is the importance of meticulous preoperative planning. Advanced imaging techniques, such as 3D vascular mapping and dynamic MRI, can reveal hidden anatomical variations that might sway the decision toward ALIF or TLIF. For example, a patient with borderline vascular structures might benefit more from a minimally invasive TLIF, reducing the risk of vascular injury. This tailored approach underscores the evolution from a one-size-fits-all mindset to a truly personalized surgical plan.
How Do Surgeon Experience and Technique Evolution Impact Outcomes?
Over the years, I’ve observed that surgeon experience with minimally invasive and robotic-assisted techniques significantly influences success rates. Surgeons well-versed in the latest innovations tend to navigate anatomical challenges with greater precision, minimizing complications. A recent article I read, here, emphasizes that integrating robotic systems can enhance accuracy, especially in complex cases. Personally, I believe that choosing a surgeon who actively adopts these advancements reflects a commitment to optimizing patient outcomes.
What Are the Long-Term Considerations Beyond Fusion Success?
While immediate pain relief and fusion rates are crucial, I’ve come to appreciate the importance of understanding long-term biomechanical effects. Fusion alters natural spinal motion, potentially leading to adjacent segment degeneration—a phenomenon I find both fascinating and concerning. Discussions with my surgeon about motion-preserving alternatives, such as disc replacements, opened my eyes to future possibilities. Exploring these options requires a comprehensive understanding of the risks, benefits, and how they align with individual patient goals.
Are There Emerging Technologies That Could Redefine the Future of Spinal Surgery?
Indeed, the horizon is bright with innovations. From bioengineered grafts to augmented reality-assisted surgeries, the field is rapidly advancing. I’ve been particularly intrigued by the potential of robotic-assisted spine surgery, which promises increased precision and reduced recovery times. As a patient and observer, I believe embracing these technologies can elevate standards and personalize spine care even further.
If you’re contemplating spinal fusion or other complex procedures, I encourage you to delve into these evolving areas, ask your surgeon about their experience with new techniques, and consider how emerging innovations might benefit you. Sharing your experiences or questions below can foster a community of informed, empowered patients on their healing journeys.
The Nuances of Preoperative Planning in Spinal Fusion
My journey into spinal fusion extended beyond understanding the basic procedures. I quickly realized that meticulous preoperative planning is paramount. Cutting-edge imaging technologies, such as 3D vascular mapping and dynamic MRI, unveil subtle anatomical variations that significantly influence surgical strategy. For example, a patient with borderline vascular structures might be a candidate for minimally invasive TLIF, reducing vascular injury risk. This personalized approach exemplifies the shift from generic to tailored surgical plans, emphasizing that every detail counts when aiming for optimal outcomes.
The Impact of Surgeon Experience and Technological Evolution
Over the years, I observed how surgeon expertise, especially with minimally invasive and robotic-assisted techniques, dramatically affects success rates. Surgeons who integrate innovations like robotic systems can navigate complex anatomies with precision, minimizing complications. A notable study highlights that robotic-assisted spine surgery enhances accuracy, especially in challenging cases (see here). Personally, I believe that choosing a surgeon committed to continuous learning and technological adoption is crucial for achieving the best possible outcomes.
Long-term Biomechanical Consequences and Future Technologies
While immediate fusion success is vital, understanding long-term biomechanical alterations is equally important. Fusion alters spinal dynamics, potentially leading to adjacent segment degeneration, a phenomenon I find both intriguing and concerning. Discussions with my surgeon about alternatives like disc replacements opened my eyes to innovative solutions that preserve motion. Emerging technologies, such as bioengineered grafts and augmented reality-assisted surgeries, are poised to revolutionize the field (explore here). These advancements promise more personalized, less invasive options that could redefine spinal care for future generations.
What Advanced Techniques Should I Consider for Optimal Outcomes?
In my experience and research, embracing robotic-assisted procedures and motion-preserving technologies can significantly improve results. These innovations enhance precision, reduce recovery time, and minimize complications. If you’re contemplating spinal fusion, I encourage you to consult with surgeons experienced in these techniques and ask about their adoption of the latest tools. Engaging with credible sources and sharing your questions below can help you navigate this complex decision-making process more confidently. Remember, staying informed about technological progress and personalized approaches is key to achieving the best long-term health for your spine.
Things I Wish I Knew Earlier (or You Might Find Surprising)
The Power of Personalized Planning
One surprising insight I discovered is how critical detailed preoperative planning is. Advanced imaging like 3D vascular mapping can reveal hidden anatomical nuances, helping tailor the best approach for each patient. It’s a reminder that no two spines are exactly alike, and personalized assessments can make a real difference in outcomes.
The Impact of Surgeon Experience and Tech Innovation
Over time, I realized that a surgeon’s familiarity with cutting-edge techniques, such as robotic-assisted surgery, can dramatically influence success rates. Choosing a specialist who embraces innovations means benefiting from more precise procedures and potentially faster recovery.
Long-Term Biomechanical Effects Matter
I was surprised to learn how spinal fusion can affect future mobility and lead to adjacent segment degeneration. It’s essential to discuss long-term implications with your surgeon and explore options like disc replacement that preserve motion, aligning treatment with your lifestyle goals.
Understanding the Risks—And How to Manage Them
From my experience, being fully aware of risks like nerve injury or infection is vital. Engaging in open conversations with your surgeon and verifying their credentials can build confidence and help manage expectations effectively.
The Role of Emerging Technologies
Emerging innovations, including bioengineered grafts and augmented reality, are poised to revolutionize spine surgery. These advancements aim to enhance precision, reduce recovery times, and offer more personalized care—exciting prospects for future patients.