Unraveling the Hidden Risks of Spinal Hardware in New Jersey Back Surgery
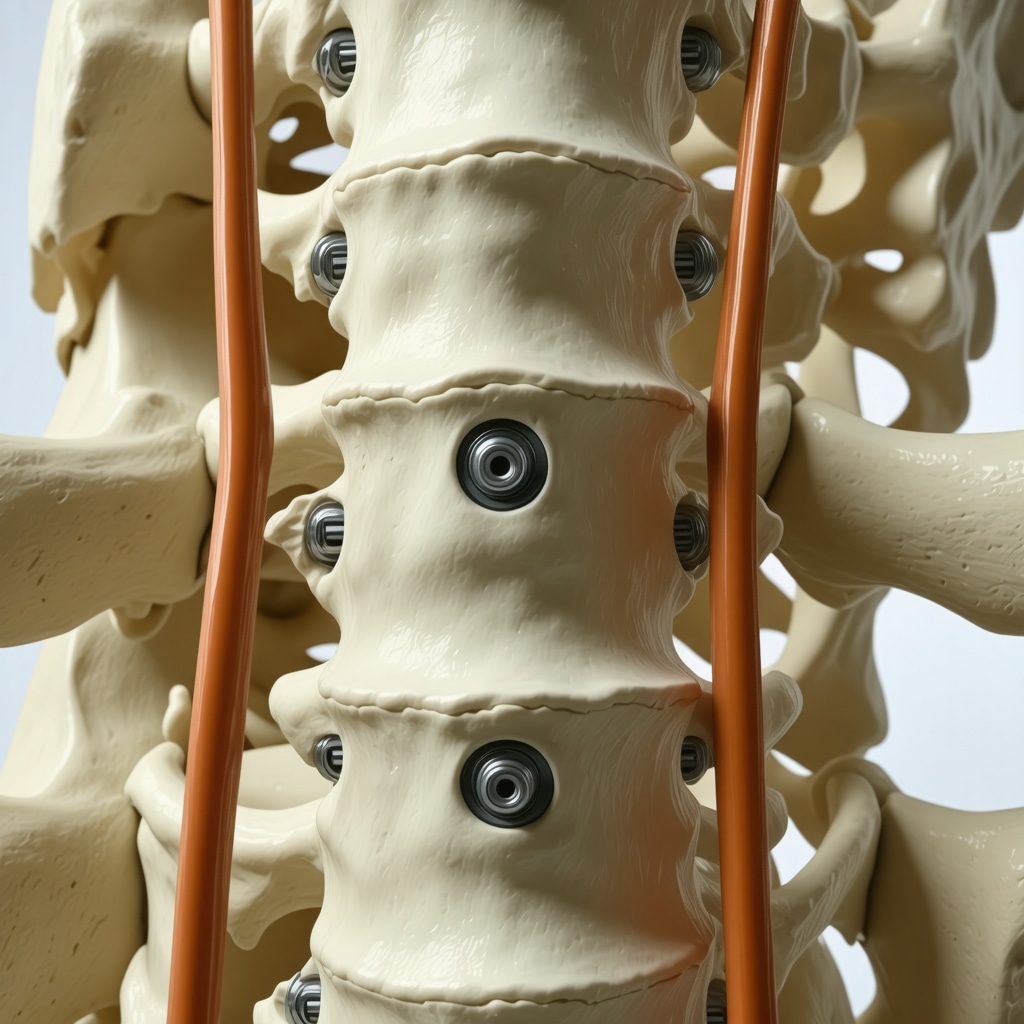
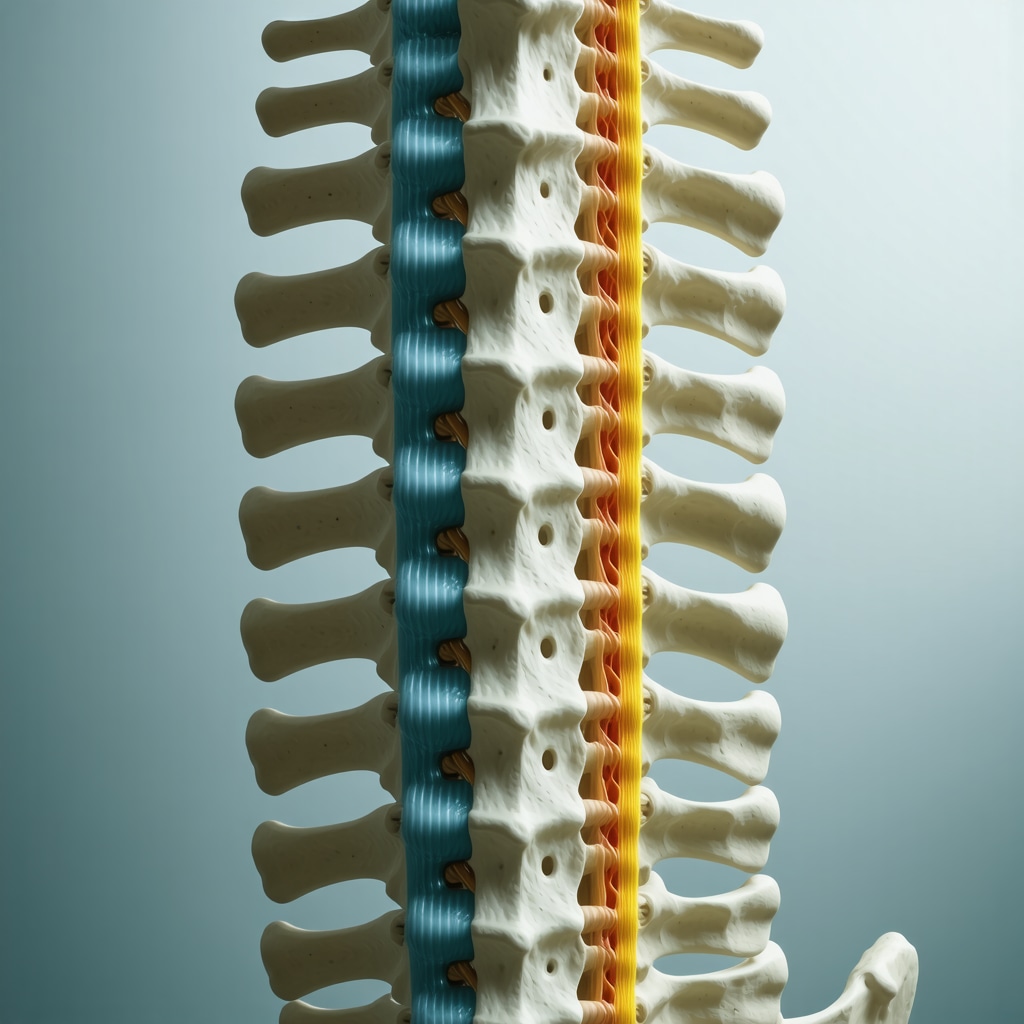
Back surgery involving spinal hardware is a pivotal intervention for many patients in New Jersey, offering relief from debilitating pain and restoring spinal stability. However, the presence of implants such as rods, screws, and plates introduces potential complications that require careful understanding. Navigating these risks is crucial for patients and clinicians alike to optimize outcomes and minimize adverse effects.
When Stability Becomes a Double-Edged Sword: The Complexities of Spinal Implant Complications
Spinal hardware aims to stabilize vertebrae after procedures like spinal fusion, yet complications can arise including hardware loosening, migration, or even breakage. These issues may lead to persistent pain, nerve irritation, or impaired mobility. For instance, a patient undergoing lumbar fusion in New Jersey might experience screw loosening months post-surgery, necessitating revision surgery. Such scenarios underscore the importance of meticulous surgical technique and postoperative monitoring.
How Do NJ Spine Surgeons Identify and Manage Hardware-Related Issues Post-Back Surgery?
Expert spine surgeons in New Jersey employ a combination of clinical evaluation and advanced imaging techniques like CT scans or MRIs to detect hardware complications early. Symptoms such as new onset of localized pain, swelling, or neurological deficits prompt thorough assessment. Management strategies range from conservative approaches, including physical therapy and medication, to surgical revision when hardware failure threatens spinal integrity. Multidisciplinary care ensures tailored treatment plans that align with patient-specific factors.
Innovations in NJ Spine Surgery: Minimizing Hardware Risks Through Advanced Techniques
The evolution of spinal surgery in New Jersey incorporates minimally invasive methods and robotic-assisted technologies, reducing tissue disruption and enhancing hardware placement precision. These advancements contribute to lowering complication rates and expediting recovery. For patients interested in the latest surgical innovations, resources such as robotic-assisted spine surgery insights offer comprehensive information on cutting-edge procedures.
Practical Experience: Real Patient Journeys Through Spinal Hardware Challenges
Consider the case of a middle-aged New Jersey resident who underwent cervical spine surgery with hardware implantation. Postoperative follow-up revealed subtle screw loosening detected via imaging before symptoms worsened. Prompt surgical intervention prevented neurological compromise and restored spinal stability. This example highlights the indispensable role of vigilant postoperative care and patient education to recognize early warning signs.
Understanding spinal hardware complications after NJ back surgery demands both expert knowledge and patient engagement. If you or a loved one are navigating this journey, consulting with board-certified spine specialists is paramount. Learn more about how to find certified spine surgeons in NJ and ensure your care is in expert hands.
For further reading on the risks and benefits of spinal fusion surgery, authoritative insights are available from the National Institutes of Health, providing detailed analysis on hardware-related outcomes.
If you found these expert insights valuable, please share this article with others seeking clarity on spinal surgery complications or leave a comment with your experiences and questions.
Living with Spinal Hardware: What I Wish I Knew Before and After Surgery
Reflecting on my journey through spinal surgery with hardware implantation, I realize how vital it was to manage expectations and stay well-informed. It’s not just about the surgery day; the physical and emotional recovery afterward plays an equally important role. I remember feeling anxious about potential complications but found that being proactive made all the difference. Understanding the nuances of spinal hardware, from how it supports vertebrae to recognizing symptoms that might indicate issues, helped me navigate recovery with confidence.
Why Postoperative Monitoring Feels Like a Lifeline
One lesson that stuck with me is the importance of regular follow-ups. My surgeon emphasized this early on, explaining that imaging tests like X-rays or MRIs are essential to catch any hardware-related problems before they become severe. In fact, according to the National Institutes of Health, early detection of hardware loosening or migration can prevent major complications and improve surgical outcomes. Staying committed to these checkups gave me peace of mind and helped my care team tailor my rehabilitation plan.
How Can Patients Best Advocate for Themselves During Spine Surgery Recovery?
From my experience and conversations with other patients, I’ve learned that active participation in your care is critical. Asking questions about pain management, physical therapy options, and signs of hardware issues empowers you to respond promptly if something feels off. For example, persistent pain beyond expected healing times or new neurological symptoms should never be ignored. Sharing these observations with your surgeon can make a huge difference in timely interventions.
Exploring Rehabilitation Approaches That Support Spinal Hardware Healing
Rehabilitation was a cornerstone of my recovery. It wasn’t just about rest; it involved carefully guided exercises to strengthen surrounding muscles while protecting the surgical site. In New Jersey, many spine centers offer specialized programs designed to complement surgical treatment. If you’re curious about what your rehab journey might look like, check out resources about the spine rehab process after surgery. Tailoring rehab to your specific condition and hardware type can accelerate healing and reduce risks.
Also, I found that connecting with others who underwent similar surgeries provided emotional support and practical tips. Whether through local support groups or online forums, these communities can offer insights that only fellow patients truly understand.
What Are the Common Misconceptions About Spinal Hardware That Might Surprise You?
Many people imagine spinal hardware as a permanent source of discomfort or limitation, but that’s not always the case. While some patients do face challenges like hardware irritation or rare complications, many live active, pain-free lives post-implantation. It’s important to differentiate between normal healing sensations and warning signs. Educating yourself about your specific hardware type and surgical procedure can demystify the process and reduce anxiety.
Have you or a loved one undergone spinal surgery with hardware? What was your recovery experience like? I’d love to hear your stories or questions. Sharing experiences is a powerful way to learn and support each other on this journey. Feel free to leave a comment below or explore more about finding the right certified spine surgeon in NJ to guide your care.
Decoding the Nuances of Biomechanical Stress on Spinal Implants in NJ Patients
Spinal hardware longevity hinges on understanding biomechanical forces acting upon implants post-surgery. In New Jersey, where patient lifestyles vary widely, these mechanical stresses can influence the risk of hardware fatigue or failure. Notably, axial loading, torsional forces, and repetitive micro-movements contribute to subtle implant wear that might not manifest clinically until later stages. Surgeons must integrate biomechanical principles with patient-specific activity levels to optimize implant selection and positioning, thus mitigating eventual hardware complications.
Cutting-Edge Imaging Modalities: Enhancing Early Detection of Subclinical Hardware Failures
Traditional radiographs, while valuable, have limitations in detecting early hardware issues. Advanced imaging technologies such as dynamic CT and metal artifact reduction sequence (MARS) MRI allow exquisite visualization of implant integrity and adjacent tissue reactions. These modalities enable New Jersey spine specialists to identify early signs of screw loosening, microfractures, or inflammatory responses around the implant, even before symptoms emerge. Incorporating such imaging into routine postoperative protocols elevates patient care by facilitating timely interventions.
What Are the Emerging Biomaterials Revolutionizing Spinal Hardware Durability and Biocompatibility?
Recent innovations in biomaterials have begun transforming spinal hardware design. Titanium alloys with enhanced fatigue resistance, porous-coated implants promoting osseointegration, and bioresorbable polymers reducing long-term foreign body presence represent a new frontier. These materials aim to harmonize mechanical strength with biological compatibility, decreasing risks of implant rejection or infection. Research published by the Journal of Orthopaedic Research highlights promising results of these biomaterials in preclinical and clinical settings, underscoring their potential to improve surgical outcomes significantly.
Understanding these biomaterial advancements empowers patients and providers to make informed decisions about spinal hardware options tailored to individual needs.
Integrating Multidisciplinary Postoperative Care: A Blueprint for Optimizing Hardware Success
Beyond surgical technique and material choice, multidisciplinary collaboration is paramount in managing spinal hardware outcomes. Physical therapists specializing in spine rehabilitation, pain management experts, and nutritionists contribute collectively to enhancing recovery trajectories. For instance, controlled progressive loading during rehabilitation strengthens paraspinal musculature, which offloads stress from hardware components. Nutritional optimization supports bone healing vital for implant stability. New Jersey centers adopting such comprehensive care models report improved patient satisfaction and reduced revision surgeries.
Patient education also forms a cornerstone of this approach, equipping individuals with knowledge about activity modifications and symptom vigilance.
Addressing the Psychological Dimensions of Living with Spinal Hardware
The psychological impact of spinal hardware implantation is often underappreciated. Anxiety regarding implant failure or chronic pain can exacerbate recovery difficulties. Integrating mental health support into postoperative plans—including cognitive behavioral therapy and peer support groups—can alleviate fear and improve adherence to rehabilitation. Research from the American Psychological Association emphasizes the positive outcomes of psychological interventions in orthopedic recovery.
Such holistic care models represent the future of spine surgery aftercare in New Jersey, addressing both physical and emotional well-being.
If you are preparing for or recovering from spinal surgery involving hardware, engaging with board-certified spine surgeons and exploring multidisciplinary programs can markedly enhance your outcome. For more detailed guidance, visit our expert resources on advanced spine surgery care in New Jersey.
Harnessing Biomechanical Insights to Enhance Spinal Implant Longevity
In the realm of spinal surgery, understanding the intricate biomechanical environment is indispensable for prolonging implant durability. In New Jersey, patient-specific factors such as occupational demands, physical activity, and anatomical variance profoundly influence the mechanical stresses exerted on spinal hardware. Axial compression, torsional rotation, and repetitive micromotions challenge the integrity of implants, potentially precipitating fatigue fractures or loosening. Consequently, preoperative biomechanical modeling and intraoperative navigation have become critical tools for surgeons aiming to tailor implant selection and positioning to mitigate these forces effectively.
How Are Emerging Biomaterials Transforming the Future of Spinal Hardware in NJ?
The frontier of spinal hardware innovation lies in biomaterials engineered for superior mechanical resilience and biological integration. Titanium alloys remain a gold standard due to their high strength-to-weight ratio and corrosion resistance, yet advancements such as porous titanium scaffolds promote osseointegration, enhancing implant stability. Additionally, bioresorbable polymers are gaining traction for their capacity to gradually degrade, minimizing long-term foreign body presence and reducing infection risks. A pivotal study published in the Journal of Orthopaedic Research elucidates these biomaterials’ promising roles, highlighting improved fatigue resistance and biocompatibility as key contributors to superior clinical outcomes.
Integrating Multidisciplinary Postoperative Protocols for Optimal Hardware Outcomes
Beyond surgical precision and biomaterial advancements, the postoperative phase demands a comprehensive, multidisciplinary approach to optimize spinal hardware success. Physical therapists specializing in spine rehabilitation devise progressive loading regimens that strengthen paraspinal musculature while safeguarding the surgical site, thereby reducing implant stress. Pain management specialists employ multimodal analgesia strategies to facilitate functional recovery without compromising healing. Nutritional experts contribute by ensuring adequate intake of bone-supportive nutrients such as calcium, vitamin D, and protein, which are vital for osseous integration of hardware components. Such collaborative care models, increasingly adopted in New Jersey spine centers, demonstrate marked reductions in revision surgeries and enhanced patient satisfaction.
Addressing Psychological Resilience: The Overlooked Pillar in Spinal Hardware Recovery
The psychological dimension of living with spinal hardware is often overshadowed by physical considerations, yet it plays an integral role in recovery trajectories. Anxiety surrounding implant performance or chronic discomfort can hinder rehabilitation adherence and amplify perceived pain. Incorporating mental health interventions—such as cognitive behavioral therapy and peer support networks—into postoperative care fosters resilience, mitigates fear-avoidance behaviors, and promotes holistic well-being. The American Psychological Association underscores the efficacy of such integrative approaches in enhancing orthopedic recovery outcomes.
For patients preparing for or recovering from spinal surgery with hardware, engaging with board-certified spine surgeons and embracing multidisciplinary programs can significantly elevate care quality. Discover advanced insights and personalized care pathways on our dedicated resource page Advanced Spine Surgery Care in New Jersey.
Seizing Control: Empowering Patients Through Knowledge and Proactive Communication
Active patient advocacy remains a cornerstone of optimal spinal hardware outcomes. Patients are encouraged to maintain open, detailed communication with their surgical teams, articulating any atypical symptoms such as persistent localized pain, new neurological deficits, or functional decline. Early reporting facilitates prompt diagnostic imaging and intervention, often circumventing complex revision procedures. Furthermore, staying informed about emerging biomaterials and rehabilitation protocols empowers patients to participate meaningfully in shared decision-making processes, tailoring treatment to their unique biomechanical and lifestyle contexts.
Frequently Asked Questions (FAQ)
What types of spinal hardware are commonly used in back surgery?
Spinal hardware typically includes rods, screws, plates, and cages designed to stabilize the spine after procedures such as fusion. Materials often comprise titanium alloys for strength and biocompatibility, with emerging biomaterials like porous-coated implants and bioresorbable polymers gaining traction to enhance integration and reduce complications.
How can patients recognize early signs of spinal hardware complications?
Early indications include new or worsening localized pain, swelling near the surgical site, neurological symptoms such as numbness or weakness, and decreased mobility. Prompt reporting of these symptoms to a spine surgeon enables timely diagnostic imaging and intervention to prevent severe outcomes.
What advanced imaging techniques are used to detect hardware issues?
Beyond standard X-rays, techniques like dynamic CT scans and Metal Artifact Reduction Sequence (MARS) MRI provide superior visualization of implant integrity and surrounding tissues. These modalities can identify subtle hardware loosening, microfractures, or inflammatory changes before clinical symptoms manifest.
How do biomechanical factors affect spinal implant longevity?
Biomechanical stresses such as axial loading, torsional forces, and repetitive micro-movements influence implant fatigue and potential failure. Personalized surgical planning that considers patient activity levels and anatomical variations helps optimize hardware positioning and selection to mitigate these risks.
What role do multidisciplinary teams play in postoperative care?
Multidisciplinary care involving physical therapists, pain management specialists, nutritionists, and mental health professionals enhances recovery by addressing physical rehabilitation, pain control, nutritional support for bone healing, and psychological resilience, collectively improving implant success and patient satisfaction.
Are new biomaterials truly improving spinal hardware outcomes?
Yes. Innovations such as porous titanium alloys promote osseointegration, while bioresorbable polymers reduce long-term foreign body presence and infection risk. These biomaterials improve mechanical durability and biological compatibility, translating to better clinical results as supported by recent orthopedic research.
How important is patient advocacy during recovery?
Active patient engagement is critical. Patients should communicate any unusual symptoms promptly, adhere to follow-up schedules, participate in tailored rehabilitation, and stay informed about their hardware and recovery process to enable early detection and management of complications.
Can psychological support impact recovery after spinal hardware implantation?
Absolutely. Anxiety and fear related to implant performance can hinder rehabilitation. Integrating psychological therapies like cognitive behavioral therapy and peer support networks fosters emotional resilience, improving adherence to recovery protocols and overall outcomes.
Is spinal hardware always permanent, or can implants be removed?
While spinal hardware is often intended as a permanent solution, removal may be considered in cases of persistent pain, infection, or hardware failure after the spine has sufficiently healed. Decisions are individualized based on patient condition and risk-benefit assessments.
What lifestyle adjustments help ensure the longevity of spinal hardware?
Modifying activities to avoid excessive spinal loading, adhering to rehabilitation exercises that strengthen supporting musculature, maintaining bone-healthy nutrition, and avoiding smoking contribute significantly to preserving implant integrity and function.
Trusted External Sources
- National Institutes of Health (NIH): Provides comprehensive peer-reviewed research on spinal fusion surgery outcomes, hardware complications, and best practices in postoperative care.
- Journal of Orthopaedic Research: Offers in-depth studies on biomaterials innovation, biomechanical analyses, and clinical trials advancing spinal implant technology.
- American Psychological Association (APA): Delivers evidence-based insights on psychological interventions improving orthopedic recovery and patient well-being.
- North American Spine Society (NASS): A leading professional society offering clinical guidelines, education, and research updates on spine surgery and implant management.
- New Jersey Spine Centers and Academic Medical Institutions: Local expert centers provide region-specific protocols, multidisciplinary care models, and patient resources for back surgery and spinal hardware management.
Conclusion
Spinal hardware implantation in New Jersey back surgery represents a transformative treatment for spinal disorders, yet it carries inherent risks requiring vigilant management. Understanding the complexities of biomechanical stresses, embracing cutting-edge biomaterial advancements, and committing to multidisciplinary postoperative care form the pillars of optimizing hardware longevity and patient outcomes. Equally vital is empowering patients through education and proactive communication to detect complications early and participate actively in their recovery journey. By synthesizing expert surgical techniques, innovative technologies, and holistic care approaches, spine surgeons and patients together can achieve durable, successful outcomes. If you or someone you know is considering or recovering from spinal surgery with hardware, engage with board-certified specialists and explore comprehensive rehabilitation and psychological support options. Share this article to spread awareness, comment with your experiences, and continue exploring expert content to navigate spinal health confidently and effectively.