Advanced Perspectives on Spinal Hardware Complications in Modern Surgery
In the complex field of spinal surgery, the integration of hardware such as rods, screws, and plates has revolutionized the treatment of spinal deformities and instability. However, despite technological advancements, complications related to spinal hardware remain a critical concern for both surgeons and patients. This article delves into the nuanced challenges associated with spinal hardware complications, offering insights grounded in the expertise of New Jersey spine surgeons who specialize in managing these intricate issues.
Biomechanical Challenges and Failure Mechanisms of Spinal Hardware
Spinal hardware is subjected to significant biomechanical stress that can lead to fatigue, loosening, or breakage over time. The interplay between patient-specific factors—such as bone quality, activity level, and comorbidities—and hardware design significantly influences the risk of complications. For instance, osteoporotic bone increases the likelihood of screw pullout, while high mechanical loads may precipitate rod fractures. NJ surgeons emphasize the importance of preoperative planning and intraoperative precision to mitigate these failure mechanisms, often employing advanced imaging and navigation technologies to optimize hardware placement and alignment.
What Are the Most Complex Diagnostic Challenges in Identifying Hardware-Related Issues Post-Surgery?
Diagnosing hardware complications postoperatively can be challenging due to overlapping symptoms with other spinal pathologies. Patients may present with nonspecific pain, neurological deficits, or signs of infection, necessitating a multi-modal diagnostic approach. Advanced imaging modalities including CT scans with metal artifact reduction, dynamic radiographs, and occasionally MRI are pivotal in evaluating hardware integrity and surrounding anatomical structures. NJ specialists often rely on a combination of clinical assessment and sophisticated imaging to distinguish between hardware failure, pseudoarthrosis, or adjacent segment disease, ensuring tailored interventions.
Infection Risks and the Role of Prophylaxis in Spinal Hardware Surgery
Infection remains a formidable complication in spinal hardware procedures, potentially leading to hardware colonization and subsequent removal. Prophylactic strategies, including perioperative antibiotic administration and strict aseptic techniques, are standard practice among New Jersey spine surgeons to minimize infection rates. Recent literature highlights the role of antibiotic-impregnated materials and intraoperative irrigation protocols as adjuncts to infection control. Early recognition and aggressive management of infection—often involving multidisciplinary teams—are crucial to preserving hardware function and patient outcomes (Journal of Spinal Disorders & Techniques).
Tailoring Revision Strategies: Balancing Risks and Benefits in NJ Spine Surgery
When hardware complications necessitate revision surgery, NJ surgeons adopt a patient-centric approach that weighs the risks of reoperation against potential benefits. Revision techniques vary from hardware removal and replacement to augmentation with bone grafting or use of novel fixation devices designed for enhanced biomechanical stability. Minimally invasive approaches are increasingly favored to reduce tissue disruption and accelerate recovery, as detailed in this expert review on minimally invasive spine surgery. Surgeons also consider the biological milieu and patient comorbidities to optimize fusion potential and minimize postoperative complications.
Integrating Emerging Technologies to Mitigate Hardware Complications
Robotic-assisted spine surgery and intraoperative navigation represent transformative tools in reducing hardware-related complications. NJ spine surgeons are at the forefront of adopting these technologies to enhance precision in hardware placement, decreasing malposition rates and subsequent failures. The integration of real-time feedback and three-dimensional anatomical mapping supports complex reconstructions and revisions, as discussed in this comprehensive analysis of robotic spine surgery. Such innovations exemplify the continuous evolution in managing spinal hardware challenges.
Explore More on Advanced Spine Surgery Techniques and Share Your Professional Insights
For practitioners and patients seeking deeper understanding, exploring emerging spine surgery innovations offers valuable perspectives on future directions. We invite spine care professionals to contribute their clinical experiences and discuss evolving strategies in spinal hardware management to foster a collaborative expert community.
Patient-Centered Approaches to Managing Spinal Hardware Complications
Effective management of spinal hardware complications hinges on individualized patient assessment. New Jersey spine surgeons emphasize comprehensive evaluation of patient-specific factors including age, bone density, comorbidities, and lifestyle demands. Such multidimensional assessment informs decisions regarding conservative management versus surgical revision, balancing the risks of additional intervention with functional outcomes. Evidence-based protocols integrating enhanced recovery pathways and multidisciplinary collaboration optimize patient safety and satisfaction.
Biomaterials Innovation: How Modern Hardware Designs Enhance Longevity and Compatibility
Technological advancements in biomaterials have significantly influenced spinal hardware performance. The introduction of titanium alloys, polyetheretherketone (PEEK) cages, and bioactive coatings improves biocompatibility and reduces complications such as corrosion and allergic reactions. NJ spine surgeons utilize these innovations to enhance osteointegration and minimize adverse tissue responses, thereby decreasing the incidence of hardware loosening and failure. Ongoing research into nanotechnology and smart implants promises further breakthroughs in adaptive hardware systems.
How Do Emerging Imaging Modalities Transform the Early Detection of Spinal Hardware Failures?
Advanced imaging techniques are pivotal for early identification of hardware-related complications, often before clinical symptoms manifest. Innovations such as dual-energy CT, metal artifact reduction sequences in MRI, and intraoperative 3D fluoroscopy allow for precise visualization of implant integrity and surrounding anatomical structures. NJ specialists leverage these modalities to differentiate between mechanical failures, infections, and adjacent segment degeneration, facilitating timely and targeted interventions that improve prognosis. For an in-depth review on imaging advancements, see the Radiographics journal article on spinal implant imaging.
Multidisciplinary Collaboration: Integrating Pain Management and Rehabilitation in Hardware Complication Care
Addressing spinal hardware complications extends beyond surgical correction to encompass comprehensive pain management and rehabilitation. NJ spine centers adopt a multidisciplinary approach involving anesthesiologists, physical therapists, and pain specialists to tailor post-revision care. Modalities such as nerve blocks, neuromodulation, and customized physical therapy regimens support functional recovery and reduce chronic pain risks. This holistic strategy aligns with current best practices for improving long-term outcomes and quality of life.
Legal and Ethical Considerations in Spinal Hardware Revision Surgery
Revision surgeries for spinal hardware complications entail legal and ethical challenges, particularly regarding informed consent and risk disclosure. NJ spine surgeons prioritize transparent communication about potential complications, alternative treatments, and expected outcomes. Furthermore, documentation and adherence to evidence-based guidelines safeguard both patient rights and practitioner accountability. Resources such as legal spine evaluations in NJ provide critical frameworks for navigating these complexities.
Join the Discussion: Share Your Experiences and Insights on Managing Spinal Hardware Challenges
We encourage spine care professionals and patients alike to engage in dialogue regarding innovative strategies and real-world experiences in spinal hardware complication management. Sharing insights fosters a collaborative environment that advances clinical practice and patient education. For further reading on minimally invasive techniques that reduce hardware-related complications, explore this detailed resource. Your comments and shared expertise are invaluable to the evolving spine care community.
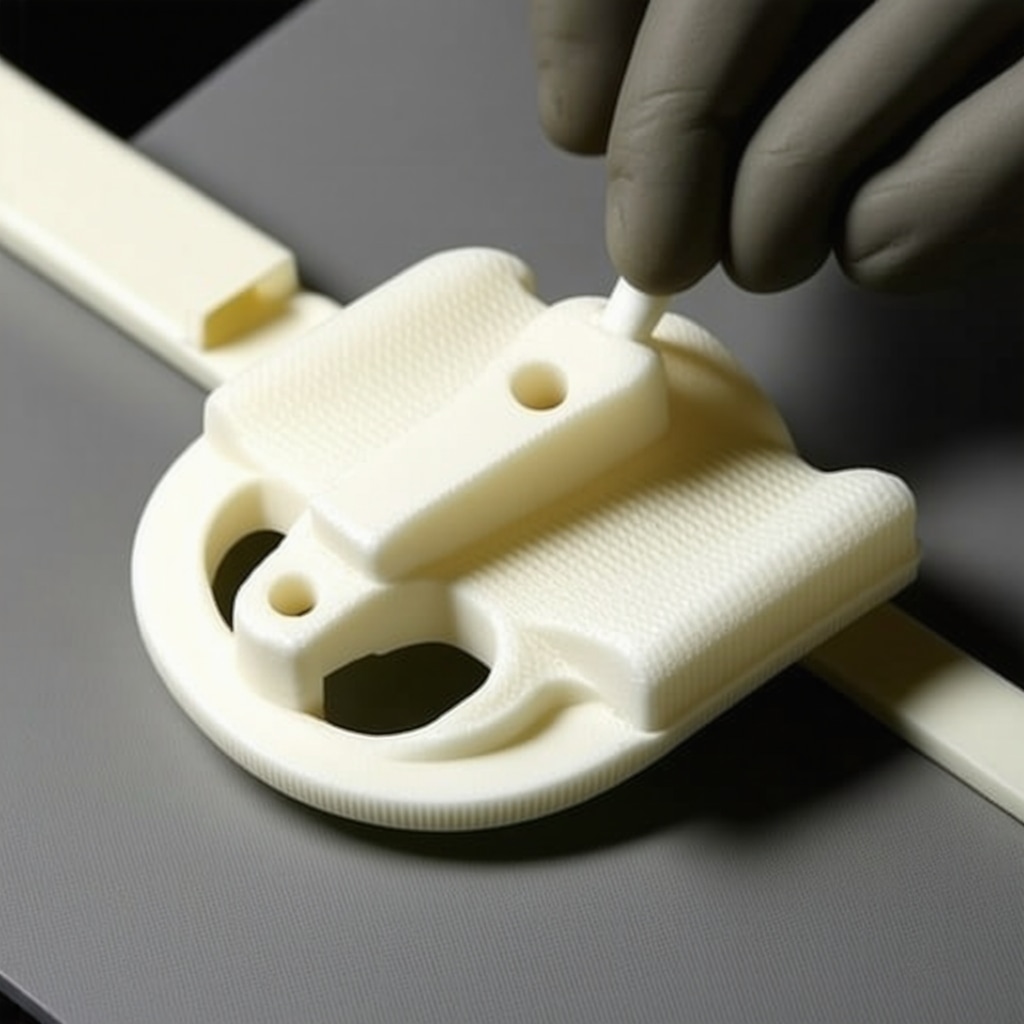
Precision in Revision Surgery: Leveraging Patient-Specific Instrumentation and Custom Implants
Revision spinal surgery to address hardware complications demands unparalleled precision due to altered anatomy, scar tissue, and compromised bone stock. New Jersey spine surgeons are increasingly harnessing patient-specific instrumentation (PSI) derived from preoperative 3D imaging and computer-aided design to tailor implants and guides uniquely suited to an individual’s anatomy. This bespoke approach minimizes intraoperative guesswork, reduces operative time, and enhances hardware stability by ensuring optimal screw trajectories and implant fit. The integration of additive manufacturing (3D printing) enables rapid production of custom cages and fixation devices that conform precisely to irregular bone surfaces, providing superior biomechanical support in complex revision cases.
What Criteria Guide the Selection of Custom Versus Standard Hardware in Complex Revision Procedures?
Determining when to utilize custom implants over standard hardware hinges on multiple factors, including the extent of bone loss, the presence of deformity, and patient-specific biomechanical demands. Surgeons evaluate the quality and quantity of residual bone via high-resolution CT scans and assess the feasibility of standard instrumentation to achieve mechanical stability. Custom implants become indispensable when conventional devices cannot accommodate anatomical irregularities or when prior hardware failure has significantly compromised native bone. NJ experts emphasize multidisciplinary planning involving engineers and radiologists to optimize implant design and ensure long-term success.
Harnessing Artificial Intelligence and Machine Learning for Predictive Analytics in Hardware Complication Risk
The advent of artificial intelligence (AI) and machine learning (ML) is poised to revolutionize preoperative risk stratification for spinal hardware complications. By analyzing vast datasets encompassing patient demographics, comorbidities, bone density metrics, and surgical variables, AI algorithms can predict individuals at elevated risk for hardware failure, infection, or nonunion. This predictive capability enables surgeons to personalize surgical planning, select appropriate hardware, and implement targeted perioperative interventions. New Jersey spine centers are actively participating in clinical trials to validate these models, aiming to enhance decision-making precision and reduce complication rates.
Exploring the Role of Bioactive and Resorbable Materials in Next-Generation Spinal Hardware
Recent biomaterial innovations focus on bioactive coatings and resorbable implants that promote osteogenesis while minimizing long-term complications associated with permanent hardware. For example, hydroxyapatite and calcium phosphate coatings enhance bone-implant integration, reducing micromotion and loosening. Concurrently, bioresorbable polymers and magnesium-based alloys offer the potential to provide temporary stabilization during fusion, subsequently degrading to eliminate the need for removal surgery. While promising, these materials require rigorous clinical evaluation to confirm their mechanical reliability and biocompatibility. NJ surgeons collaborate with biomaterials researchers to pioneer these advancements, integrating translational science into clinical practice.
Optimizing Postoperative Surveillance: Integrative Protocols Combining Advanced Imaging and Biomarker Monitoring
Early detection of hardware complications is critical to prevent catastrophic failure and optimize outcomes. Emerging protocols in New Jersey incorporate a multimodal surveillance strategy combining periodic advanced imaging modalities with biomarker analysis. Techniques such as dual-energy CT with metal artifact reduction enable detailed assessment of hardware integrity and periprosthetic bone changes. Simultaneously, serum and synovial fluid biomarkers indicative of inflammation or infection, including C-reactive protein and procalcitonin, provide real-time physiological insights. Integrating these data streams into centralized platforms facilitates timely clinical decision-making and individualized patient follow-up.
How Can Machine Learning-Driven Imaging Analytics Enhance Early Diagnosis of Hardware Loosening?
Machine learning algorithms applied to imaging datasets can detect subtle patterns of hardware loosening before overt clinical manifestations. By quantifying micro-movements, periprosthetic radiolucency, and bone remodeling dynamics, these tools offer sensitive and specific markers for impending failure. NJ radiologists collaborate closely with spine surgeons to implement AI-driven workflows that augment traditional interpretation, thereby expediting intervention and reducing morbidity. For comprehensive insights into this emerging field, refer to the seminal study on AI applications in musculoskeletal implant imaging.
Decoding AI-Enhanced Predictive Models for Personalized Hardware Surveillance
Artificial intelligence’s integration into spinal hardware management transcends conventional diagnostics, ushering in an era where predictive analytics guide individualized care. Advanced machine learning frameworks analyze multidimensional patient data—including bone mineral density, genetic markers, and biomechanical load patterns—to stratify complication risks with unprecedented accuracy. This nuanced risk profiling informs bespoke surgical planning and postoperative monitoring, enabling preemptive adjustments that mitigate failure probabilities. New Jersey spine centers exemplify this paradigm shift, fostering collaborations between data scientists and clinicians to refine algorithmic precision and clinical applicability.
How Do AI-Driven Predictive Tools Influence Surgical Decision-Making in Complex Revision Spine Cases?
In complex revision scenarios, AI-driven predictive tools synthesize heterogeneous clinical variables to forecast hardware failure trajectories and fusion likelihood, thus empowering surgeons to tailor implant selection and operative strategies. These tools integrate imaging analytics with patient-specific biomechanical simulations, facilitating dynamic risk-benefit assessments that optimize hardware configuration and minimize reoperation rates. The precision afforded by these predictive models supports adaptive intraoperative decision-making, enhancing patient outcomes in high-stakes revision procedures.
Nanotechnology and Bioactive Coatings: Elevating Hardware Osteointegration and Longevity
Emerging nanotechnology applications in spinal hardware design focus on bioactive surface modifications that stimulate cellular adhesion, proliferation, and differentiation at the bone-implant interface. Nanostructured coatings, such as titanium dioxide nanotubes and graphene composites, exhibit enhanced osteoconductivity and antimicrobial properties, reducing biofilm formation and infection risks. These innovations not only prolong implant lifespan but also expedite fusion processes, particularly in osteoporotic or compromised bone environments. Ongoing clinical trials in New Jersey assess the translational impact of these materials on patient-centric outcomes.
Augmenting Hardware Stability: Innovations in Load-Sharing and Smart Implant Systems
Smart spinal implants embedded with microelectromechanical sensors enable real-time monitoring of biomechanical stresses and micro-movements, providing continuous feedback on hardware integrity. These systems facilitate early detection of mechanical fatigue and loosening, prompting timely clinical interventions. Additionally, novel load-sharing designs distribute axial and torsional forces more evenly, mitigating stress concentration points that predispose to implant failure. NJ surgeons are pioneering these technologies, integrating sensor data with surgical navigation platforms to enhance intraoperative precision and postoperative surveillance.
Bridging Biomarkers and Imaging: A Synergistic Approach for Early Hardware Complication Detection
The convergence of molecular biomarkers and advanced imaging modalities heralds a new frontier in spinal hardware complication surveillance. Biomarkers such as interleukin-6, tumor necrosis factor-alpha, and matrix metalloproteinases serve as early indicators of localized inflammation or osteolysis. Coupling biomarker assays with high-resolution modalities like dual-energy CT and metal artifact reduction MRI enhances diagnostic specificity, facilitating differentiation between aseptic loosening and infection. This integrative approach, adopted by top NJ spine centers, optimizes timing and selection of therapeutic interventions.
Ethical Dimensions of AI Integration in Spine Surgery: Navigating Data Privacy and Clinical Accountability
The deployment of AI in spinal hardware management introduces complex ethical considerations regarding patient data stewardship, algorithmic transparency, and decision-making accountability. NJ spine surgeons advocate for rigorous governance frameworks that ensure informed consent encompasses AI-assisted diagnostics and interventions. Transparent validation of AI models is critical to maintain clinical trust and mitigate biases that could adversely affect vulnerable populations. Institutions emphasize interdisciplinary oversight committees to uphold ethical standards while fostering innovation.
Explore Cutting-Edge Insights and Collaborate on Advancing Spinal Hardware Solutions
For spine care specialists dedicated to pushing the boundaries of spinal hardware complication management, engaging with the latest research and clinical innovations is imperative. We invite you to delve deeper into AI applications and biomaterial advancements by visiting the National Institutes of Health’s comprehensive review on AI and biomaterials in orthopedic implants. Join the conversation to exchange expertise and shape the future of personalized spinal surgery.
Expert Insights & Advanced Considerations
Nuanced Biomechanical Evaluation is Paramount in Hardware Longevity
Understanding the complex interplay between patient-specific biomechanics and implant design is critical. New Jersey spine surgeons stress that preoperative assessment of bone quality and mechanical loading patterns informs optimal hardware selection and placement, thus mitigating risks of fatigue failure and loosening.
Integration of AI and Machine Learning Enhances Predictive Risk Stratification
AI-driven analytics empower clinicians to anticipate hardware complications by analyzing multifactorial data sets encompassing patient demographics, surgical variables, and imaging findings. This predictive foresight facilitates personalized surgical planning and targeted prophylactic interventions, reducing revision rates in complex cases.
Custom Implants and Patient-Specific Instrumentation Elevate Revision Surgery Outcomes
Tailoring hardware through 3D imaging and additive manufacturing addresses anatomical challenges and compromised bone stock in revision surgeries. This bespoke approach minimizes operative time and enhances implant stability, a practice increasingly adopted by NJ experts in complex spinal reconstructions.
Multimodal Surveillance Combining Biomarkers and Advanced Imaging Optimizes Early Detection
Combining serum inflammatory markers with cutting-edge imaging modalities like dual-energy CT and metal artifact reduction MRI offers a synergistic strategy for early identification of infection or mechanical failure, enabling timely intervention and improved patient prognosis.
Ethical Frameworks Must Evolve Alongside Technological Advances in AI-Assisted Care
As AI integration deepens, NJ spine centers emphasize the importance of transparent patient communication, informed consent, and algorithmic accountability to uphold ethical standards and maintain trust in technologically augmented surgical decision-making.
Curated Expert Resources
National Institutes of Health (NIH) Review on AI and Biomaterials in Orthopedic Implants: An authoritative source detailing the latest innovations in AI applications and biomaterial science relevant to spinal hardware advancements.
Journal of Spinal Disorders & Techniques: Provides peer-reviewed research on infection prophylaxis and advanced surgical techniques, essential for understanding hardware complication management.
Radiographics Journal Article on Spinal Implant Imaging: Offers in-depth analysis of advanced imaging modalities critical for accurate diagnosis of hardware failures.
NJ Spine Surgeons Online Resources: Comprehensive guides such as Minimally Invasive Spine Surgery Benefits and Robotic-Assisted Spine Surgery Future or Fad offer localized expert perspectives and evolving treatment modalities.
Legal Spine Evaluations in NJ: A crucial resource outlining the medico-legal considerations and patient rights relevant to spinal hardware revision surgeries.
Final Expert Perspective
Spinal hardware complications represent a multifaceted challenge requiring a synthesis of biomechanical insight, cutting-edge technology, and ethical vigilance. The integration of AI predictive models, patient-specific implant customization, and comprehensive surveillance protocols is reshaping the landscape of spinal surgery in New Jersey. Embedding these advancements within patient-centered frameworks ensures not only enhanced hardware longevity but also improved clinical outcomes and patient satisfaction. For those invested in advancing spinal care, engaging with ongoing research and collaborative discourse is vital. To deepen your understanding and connect with NJ’s leading experts, explore additional resources such as Choosing the Best Spine Surgeon in NJ and Top Spine Surgery Techniques to Watch in 2025. Your professional insights and engagement contribute meaningfully to the evolution of spinal hardware complication management.


The article does a remarkable job highlighting the intricate balance required in spinal hardware management. From my perspective, what stands out is the emphasis on patient-specific factors such as bone quality and activity levels influencing hardware failure risks. In particular, the detailed discussion on advanced imaging for diagnosing hardware complications resonates with challenges I’ve observed in clinical settings where symptoms overlap with other spinal conditions. The integration of technologies like robotic-assisted surgery and AI-driven predictive models truly seems transformative. It’s fascinating how NJ surgeons are leveraging these advancements not only to improve hardware placement accuracy but also to anticipate and mitigate potential failures before they manifest clinically.
One aspect I find particularly compelling is the move toward customized implants via 3D printing, which seems key when conventional hardware falls short, especially in revision surgeries with compromised bone stock. However, I wonder about the accessibility and cost-effectiveness of such personalized solutions on a wider scale. Also, the article’s point on multidisciplinary approaches encompassing pain management and ethics adds important depth to patient care.
Has anyone else experienced significant improvements in patient outcomes through AI-assisted surgical planning or custom implants in spinal hardware cases? What are the main hurdles you’ve encountered when integrating these innovations in everyday practice?
Reading this detailed overview on spinal hardware complications truly highlights how far our field has come with technology integration. In my practice, I’ve seen firsthand how advanced imaging modalities, especially metal artifact reduction CT, have significantly improved our ability to diagnose hardware loosening early, often before symptoms become severe. I also concur with the emphasis on personalized, patient-specific approaches—particularly in complex revision cases—where 3D printing of custom implants can dramatically improve outcomes.
One challenge I’ve encountered is balancing the cost and accessibility of these cutting-edge solutions with wider patient populations. It’s exciting but also raises questions about how we can make these innovations more universally available. I am curious—what strategies have others found effective in overcoming resource limitations to implement such sophisticated technologies? Additionally, with AI and machine learning being more prevalent, how do you see ethical considerations evolving, especially regarding data privacy and decision-making transparency? It seems vital that as we develop these tools, we maintain a focus on ethical standards to support patient trust and safety.
This comprehensive review really underscores how critical personalized approaches are when it comes to complex spinal hardware cases. From my experience, integrating advanced imaging techniques like dual-energy CT has been a game-changer in early detection of potential failures, often before clinical symptoms surface. I’ve also seen the positive impact of patient-specific implants created through 3D printing in revision surgeries, especially in cases with significant bone loss. It seems like these technological advancements are paving the way for more predictable outcomes, which is promising.
This post provides a comprehensive look at the complexities involved in managing spinal hardware complications. From my clinical experience, I’ve observed that integrating emerging technologies such as AI-driven predictive analytics and custom 3D-printed implants truly enhances surgical precision and patient outcomes. One challenge I’ve faced is ensuring these advanced solutions are accessible to a broader patient demographic, given their costs. I wonder how other practitioners are addressing resource limitations while still adopting cutting-edge innovations. Additionally, the discussion on nanotechnology coatings and smart implants excites me—do you think these will become standard in the next decade? Overall, the emphasis on personalized, multidisciplinary care aligns well with the future of spine surgery, fostering both safety and durability.