Unlocking the Mystery: What Exactly Is Spinal Stenosis Surgery?
Spinal stenosis surgery is a specialized procedure designed to relieve the pressure caused by narrowing spaces within your spine, which can compress the nerves traveling through it. This condition often leads to debilitating pain, numbness, or weakness, particularly in the lower back and legs. Understanding this surgery requires more than just knowing its name; it involves delving into the complexities of spinal anatomy and the nuanced decision-making behind surgical intervention.
The Anatomy of Relief: How Spinal Stenosis Surgery Alleviates Nerve Compression
At its core, spinal stenosis surgery aims to create more space for the spinal cord and nerve roots. There are several surgical techniques, such as laminectomy, laminotomy, and spinal fusion, each tailored to the patient’s specific condition. For example, a laminectomy involves removing a portion of the vertebral bone called the lamina to decompress the nerves. In contrast, spinal fusion might be necessary if instability accompanies stenosis, fusing adjacent vertebrae to provide stability.
These procedures are often performed after conservative treatments fail to provide lasting relief, and the patient’s quality of life is significantly affected. The choice of technique depends on factors like the stenosis location, severity, and patient health.
How Do Surgeons Decide If You’re a Candidate for Spinal Stenosis Surgery?
Determining candidacy for spinal stenosis surgery requires a multidisciplinary approach. Experts evaluate symptoms, physical examination findings, and imaging studies such as MRI or CT scans to assess the degree of nerve compression. Surgeons also weigh risks versus benefits, considering patient age, comorbidities, and lifestyle.
Often, patients undergo a trial of conservative care—including physical therapy, medications, and injections—before surgery is recommended. The decision is deeply personalized, aiming to optimize outcomes and minimize complications. More information on identifying when surgery might be necessary can be found in Signs You Might Need Spinal Surgery: Expert Insights.
Innovations in Spinal Stenosis Surgery: From Traditional to Minimally Invasive Techniques
Recent advances have revolutionized spinal stenosis surgery. Minimally invasive spine surgery (MISS) techniques, for instance, use smaller incisions and specialized instruments to reduce tissue damage, leading to quicker recovery and less postoperative pain. Procedures like endoscopic decompression exemplify this shift, allowing surgeons to precisely target the stenotic area.
Moreover, robotic-assisted spine surgery is gaining traction, offering enhanced precision and potentially better outcomes. For a deeper dive into modern surgical techniques, including robotic assistance, explore Robotic-Assisted Spine Surgery: Future or Fad?.
Real Patient Experiences: Navigating Life Before and After Spinal Stenosis Surgery
Consider Jane, a 62-year-old avid gardener who struggled with chronic leg pain and numbness that limited her daily activities. After exhaustive conservative treatment, her surgeon recommended a laminectomy. Post-surgery, Jane experienced significant relief and regained her mobility, returning to the garden she loved. Stories like Jane’s highlight the transformative potential of spinal stenosis surgery when carefully selected and expertly performed.
Patients’ experiences underscore the importance of thorough preoperative evaluation and postoperative rehabilitation, which are critical for maximizing benefits and maintaining spinal health.
Where Can You Find Trusted Expertise for Spinal Stenosis Surgery?
Choosing the right surgeon is paramount. Board-certified spine surgeons bring extensive training and experience to the table, ensuring the best possible care. To find qualified specialists near you, consider resources like How to Find Board-Certified Spine Surgeons Near You.
For personalized consultation or to explore your treatment options further, don’t hesitate to contact a spinal care professional who can guide you through the complexities of spinal stenosis surgery.
Curious about the Recovery Process After Spinal Stenosis Surgery?
Recovery varies depending on the surgical approach and individual patient factors. Generally, patients can expect several weeks to months of rehabilitation, including physical therapy to restore strength and flexibility. Pain management and lifestyle adjustments are also integral parts of recovery. Engaging actively in postoperative care often determines long-term success.
For a comprehensive overview of surgical options and recovery considerations, visit Exploring Minimally Invasive Spine Surgery Benefits.
If you found these insights helpful, consider sharing this guide to help others navigating spinal stenosis.
For authoritative information on spinal stenosis and related surgical treatments, the National Center for Biotechnology Information provides a detailed review of surgical outcomes and indications.
Adjusting to Life Post-Surgery: My Unexpected Journey
Reflecting on my own experience with spinal stenosis surgery, I remember the mix of relief and uncertainty that accompanied my recovery. Initially, the pain that had overshadowed daily life faded, but new challenges emerged—learning how to move without overstraining, managing fatigue, and embracing a slower pace. It was a humbling reminder that surgery is not a quick fix but rather a step in a longer healing process.
One unexpected lesson was the importance of patience. I found that celebrating small milestones, like walking a little farther each day or sitting comfortably without pain, made a huge difference in maintaining motivation. It also helped to lean on my support system—family, friends, and healthcare providers—who offered encouragement and practical help.
How Can You Balance Activity and Rest During Recovery?
This question came up often during my rehabilitation. Striking the right balance between staying active enough to promote healing and resting to avoid setbacks is tricky. My physical therapist emphasized listening to my body and adjusting activity levels accordingly. For example, gentle stretching and short walks were encouraged early on, while high-impact activities were off-limits until my spine healed sufficiently.
From my research and conversations with specialists, incorporating low-impact exercises like swimming or stationary cycling can support recovery without putting undue stress on the spine. You can find more about these approaches in resources like Exploring Minimally Invasive Spine Surgery Benefits, which also discusses how minimally invasive techniques can influence the recovery timeline.
Understanding the Emotional Side of Spinal Stenosis Surgery
Physical healing is only part of the equation; the emotional journey is equally significant. It’s normal to feel frustration or anxiety when progress seems slow or when facing new physical limitations. I found journaling helpful to process these feelings and track improvements over time.
Connecting with others who have undergone similar surgeries also provided comfort and perspective. Online forums and local support groups can be great places to share stories and tips. According to a study published by the National Center for Biotechnology Information, emotional well-being can significantly impact recovery outcomes, highlighting the need for comprehensive care that addresses both mind and body.
When Should You Seek Further Medical Advice After Surgery?
Despite careful recovery, there may be moments when symptoms worsen or unexpected issues arise. If you experience increased pain, numbness, or difficulty moving, it’s crucial to consult your surgeon promptly. Early intervention can prevent complications and help adjust your treatment plan.
For those navigating these concerns, understanding the signs that warrant medical attention is essential. The article Signs You Might Need Spinal Surgery: Expert Insights offers valuable information that can also apply postoperatively in recognizing when to seek help.
Have you or a loved one undergone spinal stenosis surgery? Share your recovery tips and experiences in the comments below—your insights might be just what someone else needs to hear today.
Mastering Postoperative Rehabilitation: Strategies to Optimize Spinal Stenosis Surgery Outcomes
Postoperative rehabilitation is a critical determinant of the ultimate success following spinal stenosis surgery. Beyond the initial healing phase, a carefully curated multidisciplinary rehabilitation protocol can markedly improve functional recovery and patient satisfaction. Rehabilitation should encompass not only physical therapy but also patient education, psychological support, and lifestyle modifications.
Physical therapists specializing in spinal conditions often emphasize core stabilization exercises, proprioceptive training, and gradual reintroduction of weight-bearing activities to enhance spinal stability and prevent re-injury. Additionally, tailoring rehabilitation intensity based on intraoperative findings and the patient’s baseline functional status is vital to avoid setbacks. This personalized approach often involves advanced neuromuscular re-education techniques that facilitate improved motor control and pain modulation.
What Are the Latest Evidence-Based Protocols for Enhancing Recovery After Spinal Stenosis Surgery?
Recent studies advocate for an integrative recovery pathway that incorporates early mobilization, multimodal analgesia to minimize opioid dependence, and cognitive behavioral therapy to address psychosocial barriers to recovery. For instance, enhanced recovery after surgery (ERAS) protocols, initially designed for other surgical fields, are being adapted for spine surgery with promising results in reducing hospital stay duration and accelerating return to function.
Moreover, emerging evidence suggests that the use of neuromodulation techniques, such as transcutaneous electrical nerve stimulation (TENS), adjunct to conventional therapy, can improve postoperative pain control and functional outcomes. Engaging in tailored home exercise regimens guided by tele-rehabilitation platforms has also gained traction, enhancing patient adherence and allowing real-time monitoring by clinicians.
For an in-depth review of these cutting-edge rehabilitation strategies, refer to the comprehensive analysis published in the Journal of Orthopaedic & Sports Physical Therapy.
Decoding Long-Term Management: Preventing Recurrence and Promoting Spinal Health
Long-term success after spinal stenosis surgery hinges not only on surgical technique and immediate recovery but also on sustained spinal health and prevention of recurrent symptoms. Chronic degenerative changes and biomechanical stresses can predispose patients to future spinal issues if proactive measures are not implemented.
Patients should be counseled on weight management, ergonomic optimization, and regular low-impact aerobic exercise to maintain spinal flexibility and muscular support. Additionally, periodic clinical and radiological evaluations are prudent for early detection of adjacent segment disease or hardware complications in fusion cases.
Emerging research highlights the role of nutrition, including anti-inflammatory diets rich in omega-3 fatty acids and antioxidants, in modulating spinal tissue health and potentially mitigating degenerative progression. Integrative approaches combining physical therapy with complementary modalities such as acupuncture and mindfulness-based stress reduction may also enhance quality of life and pain management long-term.
How Can Patients Effectively Monitor and Mitigate Risks of Post-Surgical Spinal Degeneration?
Vigilant self-monitoring for symptoms like new or worsening radiculopathy, gait disturbances, or balance issues is essential. Timely consultation with spine specialists enables early intervention, which may include targeted injections, physical therapy adjustments, or, in rare cases, revision surgery.
Utilizing wearable technologies to track activity levels and spinal posture represents a frontier in proactive spinal care, empowering patients to modify behaviors dynamically. Collaborative care models involving primary care physicians, physiatrists, and spine surgeons optimize comprehensive management.
For practical guidance on sustaining spinal health post-surgery, explore resources at the Spine-Health Institute.
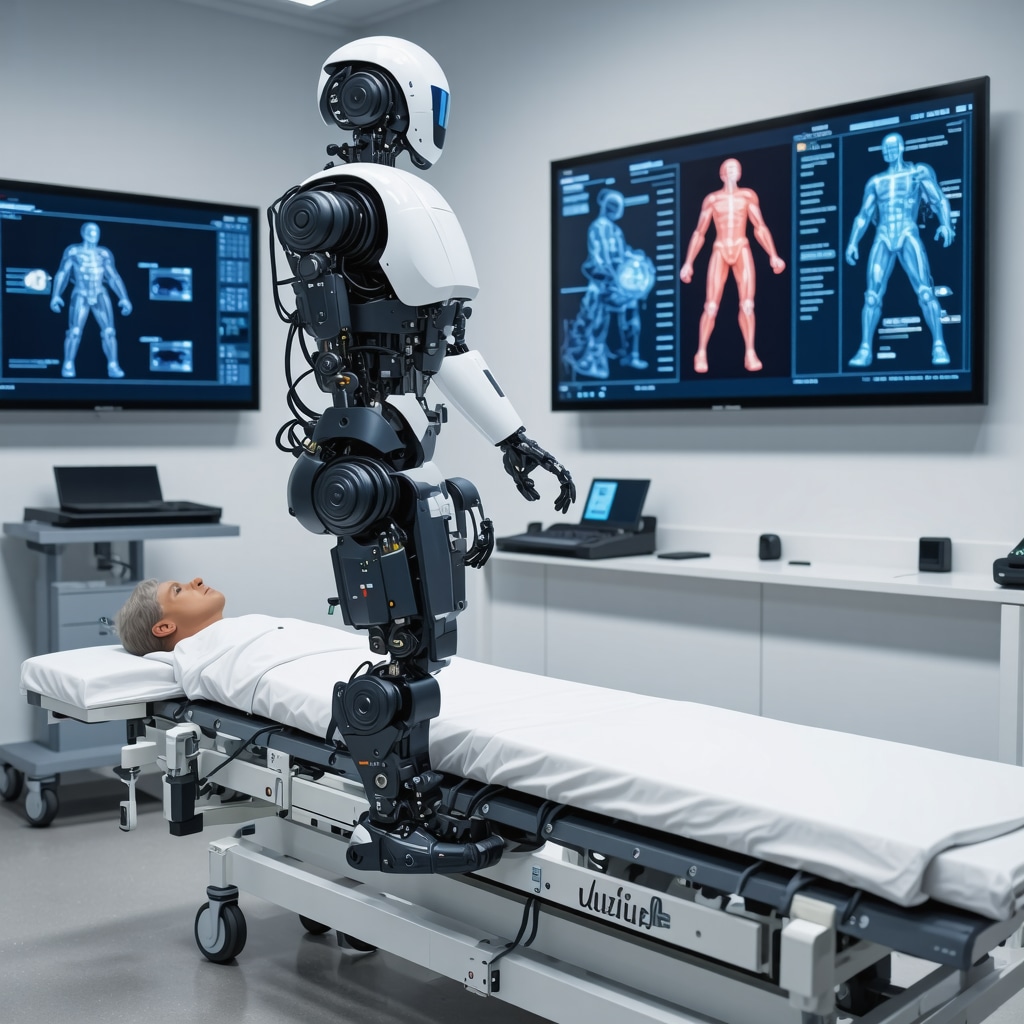
The Role of Emerging Technologies: Harnessing AI and Robotics in Post-Surgical Monitoring and Rehabilitation
Artificial intelligence (AI) and robotics are increasingly integrated into postoperative care paradigms, offering precise, data-driven insights into patient progress. AI algorithms analyze gait patterns, pain reports, and imaging data to predict complications early and personalize rehabilitation protocols.
Robotic exoskeletons and assistive devices facilitate safe mobilization, especially in patients with residual neurological deficits. These technologies not only enhance functional recovery but also reduce caregiver burden.
While still evolving, these innovations represent a paradigm shift in managing complex spinal surgery cases, promising improvements in outcomes and patient autonomy.
Are you interested in exploring how these advanced postoperative care strategies could enhance your recovery journey? Reach out to a spine care expert today for a tailored consultation.
Refining Recovery: Cutting-Edge Rehabilitation Modalities Post-Spinal Stenosis Surgery
Beyond traditional rehabilitation, recent innovations focus on integrating neuroplasticity-driven exercises and biofeedback mechanisms. These advanced modalities harness the nervous system’s inherent ability to reorganize, facilitating improved motor control and pain reduction after decompression procedures. Incorporating virtual reality (VR) based therapy, for instance, offers immersive environments that encourage patient engagement and adherence to complex movement patterns necessary for spinal stability.
Furthermore, precision rehabilitation programs increasingly utilize wearable sensor data to tailor exercise intensity and progression dynamically, optimizing outcomes while mitigating risks of overexertion. This personalized feedback loop empowers clinicians and patients alike to make data-informed decisions during the recovery continuum.
What Are the Latest Evidence-Based Protocols for Enhancing Recovery After Spinal Stenosis Surgery?
Recent studies advocate for an integrative recovery pathway that incorporates early mobilization, multimodal analgesia to minimize opioid dependence, and cognitive behavioral therapy to address psychosocial barriers to recovery. For instance, enhanced recovery after surgery (ERAS) protocols, initially designed for other surgical fields, are being adapted for spine surgery with promising results in reducing hospital stay duration and accelerating return to function.
Moreover, emerging evidence suggests that the use of neuromodulation techniques, such as transcutaneous electrical nerve stimulation (TENS), adjunct to conventional therapy, can improve postoperative pain control and functional outcomes. Engaging in tailored home exercise regimens guided by tele-rehabilitation platforms has also gained traction, enhancing patient adherence and allowing real-time monitoring by clinicians.
For an in-depth review of these cutting-edge rehabilitation strategies, refer to the comprehensive analysis published in the Journal of Orthopaedic & Sports Physical Therapy.
Long-Term Guardianship: Strategies to Prevent Recurrence and Sustain Spinal Wellness
Ensuring durable success after spinal stenosis surgery demands proactive management of biomechanical and lifestyle factors that influence spinal health. Regular engagement in low-impact aerobic activities—such as swimming, yoga, or tai chi—promotes spinal flexibility and muscular endurance without overloading vulnerable structures. Ergonomic optimization at home and workstations mitigates undue spinal strain, while weight management addresses systemic contributors to degenerative progression.
Emerging nutritional research underscores the value of diets enriched with anti-inflammatory compounds, including omega-3 fatty acids, polyphenols, and antioxidants, which may support intervertebral disc health and attenuate degenerative cascades. Complementary therapies, such as acupuncture and mindfulness-based stress reduction, not only target symptom management but also enhance overall quality of life, facilitating holistic recovery trajectories.
How Can Patients Effectively Monitor and Mitigate Risks of Post-Surgical Spinal Degeneration?
Patients are advised to maintain vigilant self-assessment for symptoms indicative of adjacent segment disease or hardware complications, such as new-onset radiculopathy, changes in gait, or balance disturbances. Early consultation with spine specialists enables timely interventions, which may include targeted injections, physical therapy adjustments, or revision surgery if necessary.
Cutting-edge wearable technologies and mobile applications now empower patients to monitor spinal posture and activity levels continuously. These devices facilitate immediate feedback and behavioral adjustments, optimizing spinal biomechanics and potentially reducing recurrence risks. Integrating multidisciplinary care teams—including physiatrists, spine surgeons, and primary care providers—ensures comprehensive surveillance and management.
For practical guidance on sustaining spinal health post-surgery, explore resources at the Spine-Health Institute.
Harnessing AI and Robotics: Pioneering the Future of Postoperative Spinal Care
The intersection of artificial intelligence (AI) and robotics is reshaping postoperative monitoring and rehabilitation paradigms. AI-driven analytics synthesize multimodal patient data—including gait metrics, pain scales, and imaging findings—to predict complications proactively and customize rehabilitation protocols. This precision medicine approach enhances patient safety and functional recovery.
Robotic exoskeletons and assistive devices provide augmented support, particularly for patients exhibiting residual neurological deficits or motor impairments. These technologies facilitate controlled mobilization, reduce fatigue, and promote neuroplasticity, thereby expediting functional gains and independence.
Though still emerging, these technologies represent a paradigm shift in managing complex spinal surgery cases, with ongoing research striving to validate efficacy and cost-effectiveness.
Are you interested in exploring how these advanced postoperative care strategies could enhance your recovery journey? Reach out to a spine care expert today for a tailored consultation.
Frequently Asked Questions (FAQ)
What exactly causes spinal stenosis, and how does it lead to nerve compression?
Spinal stenosis primarily results from degenerative changes such as osteoarthritis, disc herniation, thickening of ligaments, or congenital narrowing of the spinal canal. These changes reduce the space within the spinal canal or neural foramina, compressing nerve roots or the spinal cord itself. This compression manifests as pain, numbness, or muscle weakness, often worsening with activity.
How do surgeons determine the most appropriate surgical technique for spinal stenosis?
The choice depends on the stenosis location, severity, spinal stability, and patient-specific factors like age and overall health. For example, laminectomy removes the lamina to decompress nerves, while fusion is added when instability is present. Minimally invasive methods may be preferred for less tissue disruption. Imaging studies, clinical symptoms, and surgeon expertise guide this tailored decision.
What are the benefits and risks associated with minimally invasive spinal stenosis surgery compared to traditional open surgery?
Minimally invasive surgery (MISS) uses smaller incisions and specialized tools, resulting in reduced muscle damage, less postoperative pain, shorter hospital stays, and faster recovery. However, it requires advanced surgical skill and may not be suitable for complex or extensive stenosis. Risks include incomplete decompression or nerve injury if not carefully performed.
How long is the typical recovery period after spinal stenosis surgery, and what factors influence it?
Recovery varies widely but generally spans several weeks to months. Factors influencing recovery include the surgical technique used, patient age, preoperative fitness, presence of comorbidities, and adherence to rehabilitation protocols. Early mobilization and physical therapy are crucial for optimal outcomes.
What role does postoperative rehabilitation play in the success of spinal stenosis surgery?
Rehabilitation is vital to restore strength, flexibility, and spinal stability, reducing pain and preventing recurrence. It often includes physical therapy focusing on core stabilization, neuromuscular re-education, and gradual reintroduction of activities. Incorporating psychological support and lifestyle modifications enhances recovery and long-term spinal health.
Are there emerging technologies that improve postoperative monitoring and rehabilitation?
Yes, artificial intelligence (AI) and robotics are revolutionizing postoperative care. AI algorithms analyze patient data to predict complications and customize rehab plans, while robotic exoskeletons assist with safe mobilization and neuroplasticity. Wearable sensors and tele-rehabilitation platforms enable real-time monitoring and personalized feedback, enhancing adherence and outcomes.
How can patients prevent recurrence of spinal stenosis symptoms after surgery?
Long-term management includes maintaining a healthy weight, engaging in regular low-impact aerobic exercise, optimizing ergonomics, and following nutritional guidelines rich in anti-inflammatory foods. Periodic medical evaluations help detect early signs of degeneration or hardware issues. Patient education and integrative therapies like acupuncture or mindfulness can improve quality of life and symptom control.
When should patients seek further medical advice following spinal stenosis surgery?
Patients should promptly consult their surgeon if they experience worsening pain, new numbness, muscle weakness, gait disturbances, or balance problems. Early intervention can address complications or disease progression, potentially avoiding more invasive treatments.
How do emotional and psychological factors influence recovery after spinal stenosis surgery?
Emotional well-being significantly affects recovery trajectories. Anxiety, frustration, or depression can hinder motivation and pain management. Supportive counseling, journaling, and connecting with peer groups help patients process emotions and maintain positive engagement in rehabilitation.
Is spinal stenosis surgery a permanent solution?
While surgery often provides significant symptom relief and functional improvement, it may not be a permanent cure due to ongoing degenerative changes. Long-term success depends on surgical technique, rehabilitation, lifestyle adjustments, and proactive spinal health management to minimize recurrence and optimize quality of life.
Trusted External Sources
- National Center for Biotechnology Information (NCBI): Provides in-depth peer-reviewed articles and meta-analyses on spinal stenosis pathology, surgical outcomes, and rehabilitation strategies, ensuring evidence-based insights.
- Journal of Orthopaedic & Sports Physical Therapy (JOSPT): Offers comprehensive research on postoperative rehabilitation protocols and neuromodulation techniques relevant to spinal stenosis surgery recovery.
- Spine-Health Institute: A reputable source specializing in long-term management of spinal conditions, offering practical guidance on preventing recurrence and maintaining spinal wellness.
- American Academy of Orthopaedic Surgeons (AAOS): Authoritative resource for surgical indications, techniques, patient education, and advances in minimally invasive spine surgery.
- Society for Minimally Invasive Spine Surgery (SMISS): Provides expert information on the latest MISS techniques and technological innovations including robotic-assisted approaches.
Conclusion
Spinal stenosis surgery represents a critical intervention for alleviating nerve compression and restoring quality of life for patients with debilitating symptoms. Advances in surgical techniques, especially minimally invasive and robotic-assisted procedures, have enhanced safety and recovery. Equally important is the comprehensive postoperative rehabilitation that integrates physical, psychological, and lifestyle strategies to optimize healing and sustain spinal health.
Long-term success demands active patient engagement, vigilant monitoring, and leveraging emerging technologies like AI and robotics to personalize care. This holistic approach transforms spinal stenosis surgery from a standalone procedure into a dynamic continuum of care tailored to individual needs.
If you or a loved one are navigating spinal stenosis treatment options, we encourage you to share this guide, engage with expert resources, and consult specialized spine care professionals. Empower your recovery journey with knowledge and support to reclaim mobility and well-being.


After reading this comprehensive guide, what stands out to me is how tailored spinal stenosis surgery truly is. It’s not a one-size-fits-all approach; surgeons carefully analyze not only imaging but also the patient’s lifestyle, overall health, and specific symptoms before deciding on techniques like laminectomy or fusion. I appreciate how the article highlighted the importance of exhausting conservative treatments first—something that’s often overlooked. From my understanding, the move towards minimally invasive procedures is a game-changer, significantly reducing recovery time and postoperative pain. I also found the personal stories shared to be encouraging, especially Jane’s experience, which underlines the potential positive impact surgery can have on daily activities. One thing I’m curious about is how patients best navigate the decision between traditional open surgery and minimally invasive options when both appear viable. Are there particular factors beyond surgeon recommendation that might influence a patient’s choice? It would be interesting to hear from others who have faced this dilemma or from professionals on what patients should consider when evaluating these surgical paths. Overall, the integration of new technologies like robotic assistance seems promising for precision and safety—an exciting evolution in spine care.
Melissa, you raised an important question about navigating the choice between traditional open surgery and minimally invasive options for spinal stenosis. From what I’ve learned and observed, beyond the surgeon’s recommendation, patient lifestyle, pain tolerance, and the presence of other health conditions can heavily influence this decision. For example, for active individuals who cannot afford lengthy downtime, minimally invasive spine surgery (MISS) often provides a quicker return to function, though it might not be suitable for more complex cases requiring extensive decompression or fusion. Additionally, patient preference about incision size and recovery trajectory plays a role. Some guidelines suggest that if instability is a concern, fusion—which is more often done via open surgery—may be necessary despite longer recovery. Furthermore, access to surgeons with advanced training in MISS or robotic-assisted techniques can affect availability. I wonder how others here have balanced the potential benefits and risks when deciding on surgery type, especially when both approaches seem feasible. Has anyone found that pre-surgical rehabilitation or consultation with a multidisciplinary team helped clarify the best option? This nuanced decision really underscores the importance of personalized care in spinal stenosis treatment.
Melissa and Lucas have presented insightful perspectives on choosing between traditional open and minimally invasive spinal stenosis surgeries. Building on that, I’ve noticed from my own experience and from conversations with patients that informed patient involvement makes a significant difference. Apart from surgeon recommendations, patients often weigh recovery speed, possible post-op limitations, and their comfort with newer technologies like robotic assistance. Additionally, the psychosocial context plays a subtle yet important role—patients with strong support systems and proactive attitudes may better navigate the demands of minimally invasive approaches and postoperative rehab. Conversely, those with fewer resources might lean toward more established methods they consider more predictable. Preoperative rehabilitation and consultations with a multidisciplinary team not only clarify physical readiness but also help patients emotionally prepare, which seems crucial given the post-surgical recovery challenges described in the article. Has anyone else undergone such comprehensive pre-surgery prep, and if so, did it shape your surgical choice or recovery expectations? It would be interesting to learn how different patients balance the clinical indicators with personal life factors when making these complex decisions.
Reading through this detailed guide makes me appreciate just how complex and personalized spinal stenosis surgery really is. I’ve known a few people who opted for surgery after conservative treatments didn’t work, and the decision-making process seemed pretty overwhelming for them. It’s reassuring to see new advancements like minimally invasive techniques and robotic-assisted surgeries being integrated; they seem to offer better recovery prospects, especially for older adults or those with multiple health issues. I remember my cousin mentioning how important postoperative rehab was for her recovery, which aligns with what’s outlined here. One thing I wonder is, how do patients decide between different minimally invasive options like endoscopic decompression versus the traditional approaches? Are these choices primarily driven by surgeon expertise, or do patient preferences also play a significant role? I think that understanding all of these factors can really help people prepare mentally and physically for the journey ahead. It’s clear that a multidisciplinary approach and engaging the right specialists can make a huge difference in outcomes. I’d love to hear more about the latest patient experiences with these minimally invasive techniques—any insights or stories out there?
This article really sheds light on how individualized spinal stenosis surgery is, which is something I’ve seen firsthand. My father underwent a minimally invasive decompression procedure last year, and his recovery was surprisingly swift, mostly because the surgeon tailored the approach based on his specific stenosis location and overall health. It’s fascinating how technological advancements like robotic assistance are now playing a role in improving accuracy and outcomes. I’ve often wondered, how do patients decide between options like endoscopic decompression and more traditional methods? Do patient preferences or lifestyle factors weigh heavily in those decisions? Personally, I believe that being well-informed and engaging in thorough preoperative discussions with specialists can empower patients to make choices aligned with their goals. Has anyone here experienced a shared decision-making process that helped determine the best surgical approach for their condition? I’d be interested to hear different perspectives, especially from those who navigated complex choices or had unique considerations during their treatment.
This in-depth look at spinal stenosis surgery really reinforces how critical personalized treatment is. I had a family member recently go through a similar process, and the importance of thorough evaluation and choice of technique was clear. The advances in minimally invasive and robotic-assisted surgeries are promising, especially in reducing recovery times and complications. In my opinion, patient education and shared decision-making make a real difference in choosing the right approach. Sometimes, the fear of surgery can overshadow the potential benefits; having clear, detailed information helps setting realistic expectations. What’s your experience with managing the emotional and psychological aspects of preparing for spinal surgery? Do you think more support services could improve overall outcomes? I’d be keen to hear practical tips from others who’ve navigated this journey—particularly how they balanced their concerns with trusting their surgical team and the technology involved.
This article really resonated with me, especially the emphasis on personalized treatment and the advancements in minimally invasive techniques. I recently had a friend undergo a similar procedure, and the difference in recovery time and pain management has been remarkable. It makes me wonder, how do surgeons currently determine the best minimally invasive method for each individual? Do preoperative imaging and patient lifestyle truly guide these choices as much as they mention? Also, with the rapid development of robotic-assisted surgeries, I’m curious about how accessible these advanced options are for patients depending on where they live. I’d love to hear from others—what factors influenced your choice of technique, and what was your experience with postoperative recovery? The integration of new technologies seems promising, but as with all surgeries, the patient’s engagement and understanding seem key to successful outcomes.
Reading this comprehensive overview really highlights how much a personalized approach is crucial in spinal stenosis surgery. I’ve seen firsthand how patient-specific treatments—tailoring the surgical technique to individual anatomy and lifestyle—can dramatically improve outcomes. I had a friend who underwent a minimally invasive procedure, and her rapid recovery was impressive compared to traditional methods she researched. It makes me curious: how do surgeons incorporate patient preferences into their decision-making process? Are there specific tools or discussions that help align surgical options with patient goals? I believe that when patients are actively involved and well-informed, they tend to have better satisfaction and smoother recoveries. Also, with rapid technological advancements like robotic assistance, I wonder—how accessible are these innovations, especially in smaller or rural healthcare settings? It seems like access to the latest techniques can vary widely, impacting long-term outcomes. Would love to hear from others about their experiences navigating surgical choices and technological options.